
Rural Health Transformation Program RFI Response Analysis
Executive Summary
In preparation for meeting with state HHS secretaries, the Cicero Institute released a Request for Information seeking proposals from stakeholders on ideas of how states can best use the Rural Health Transformation Program (RHTP) funds. In total, Cicero received 24 total proposals from a variety of innovative healthcare companies. Funds for the RHTP should focus on a more technologically integrated, financially sustainable, and patient-centric healthcare model. Across the submissions, a clear focus emerged on using technology to improve access and efficiency for rural communities, including groundbreaking developments in AI and remote-patient monitoring, improving electronic health records and interoperability, and data analysis for chronic disease management. Several proposals highlight the importance of innovative payment models to ensure the financial viability of rural providers. The proposals received offer a forward-thinking vision and excellent opportunities to transform the delivery of rural healthcare.
Stakeholder-specific Analysis
AngelEye Health
AngelEye Health’s proposal is a specialized technology solution for neonatal care. It offers a technology platform that includes a camera system for family engagement, a milk-tracking system for feeding management, and a discharge coordination tool. It aims to improve outcomes for newborns in neonatal intensive care units (NICUs) and provide crucial support to rural families who often reside far from hospitals with NICUs.
Build Cities
The “Build Cities” proposal reframes a community’s engagement as a “civic, social, and economic operating system.” The platform is designed to track and verify community contributions, such as volunteering and workforce training, which can help states meet federal requirements for Medicaid Eligibility. It aims to reduce social isolation by connecting residents to healthcare institutions and to one another. By making community-led health efforts measurable, the platform can deliver and track prevention and chronic disease solutions. This approach seeks to transform rural healthcare by creating a system that integrates purpose, prevention, and participation, providing data and feedback on quality of life for providers and state leaders.
eClinicalWorks
eClinicalWorks’ proposals center on its integrated electronic health record (EHR) system. The company’s core offering is a Unified EHR Platform to streamline patient data across various care settings, a critical need for rural networks. Their proposals also highlight value-based care technologies, an AI bundle for medical note documentation, and PRISMA for data consolidation to reduce provider burnout and improve patient care coordination. The company’s focus on interoperability and efficiency is a key component of facilitating seamless data exchange between health systems.
Google Cloud
Google’s proposals focused on leveraging its cloud platform to solve systemic challenges in rural healthcare, particularly around security and data. Their rural health cybersecurity initiative offers secure technologies. Google also suggested an AI-enabled health resource platform to help rural residents find providers and provide data-driven insights to policymakers.
Harbor
Harbor’s proposal is a specialized, technology-enabled solution for remote patient monitoring (RPM). The company offers a system to monitor medically complex and post-acute patients, which is designed to reduce caregiver burnout and prevent costly hospital readmissions. Their model is designed to be financially sustainable through existing Medicaid reimbursement, offering a strong business case for hospitals to adopt their technology.
Hopscotch Primary Care
Hopscotch Primary Care’s proposals focus on an alternative payment model (APM) and a value-based care model designed to operate without Medicaid managed care organizations (MCOs). The proposal highlights a payment structure that directly compensates primary care providers for outcomes rather than services, with an emphasis on improving the health of high-risk Medicare and Medicaid populations, which are particularly prevalent in rural communities. This model is intended to reduce costs and improve health outcomes.
Nest Healthcare
Nest Health’s proposal presents a home-based, family-centered primary care model designed to eliminate structural barriers to care in rural areas. Their model utilizes a multidisciplinary team of advanced practice clinicians, nurses, behavioral health specialists, and community health workers to provide comprehensive care directly to households. The service includes 24/7 clinical access and integrates behavioral health and social needs screenings. Operating under a value-based payment model, Nest Health has demonstrated significant reductions in emergency department visits and cost savings, which it argues make the program financially sustainable beyond initial funding. This approach aims to transform rural health by improving outcomes, addressing social determinants of health, and creating local workforce development opportunities.
OnMed
OnMed’s proposal presents a unique, clinic-grade telehealth solution. It suggests installing a network of private care stations in rural community settings, such as libraries or federally qualified health centers (FQHCs). These stations would allow patients to have a live virtual visit with a clinician and include integrated diagnostics. The business model is designed to be market-based and sustainable through a combination of RHTP funding and ongoing reimbursement from various payers.
RadleyCare
RadleyCare proposes to address the behavioral health workforce crisis by becoming a large employer of peer and family support professionals for individuals with serious mental illness (SMI). They use an “Uber” and “Match.com” model to deploy mental health peer support. The proposal focuses on providing in-person and tech-enabled care that is measurement-based for accountability.
RadleyCare’s AI-driven, integrated records and communication systems are designed to address key barriers to care like access and coordination. The technology facilitates real-time communication and operational integration with the clinical care team with the goal of connecting fragmented components of the behavioral health system, including primary care and hospitals.
Syntasa
Syntasa, a partner of Google Cloud, submitted a proposal for a Rural Chronic Disease Analytics Platform (IMPACT). This solution would use data and AI to proactively identify community-level chronic illness risks, forecast future care needs, and provide insights to state leaders for data-driven decisions. The proposal focuses on using predictive analytics to shift healthcare from a reactive to a proactive model.
VSee
VSee proposes to implement a modular, market-ready digital health platform for rural hospitals and clinics. The platform features an AI Command Center that orchestrates a variety of services, including inpatient and outpatient tele-specialty care, remote patient monitoring (RPM), and hospital-at-home (HaH). This system is designed for rapid deployment and includes tools for AI-enabled documentation and predictive analytics. VSee’s goal is to expand access, improve outcomes, and lower the total cost of care for rural communities
White-label Telehealth
Chris Moose proposed white-label telehealth solutions. The proposals are geared toward empowering provider associations, health systems, and health plans to brand their own telehealth services. This is designed to be a flexible and cost-effective way for existing organizations to enter the telehealth market and expand access to care in rural areas.
CMS Category Table
To receive funding from the Rural Health Transformation Program, the Centers for Medicare and Medicaid require that states submit proposals that include three or more of the categories below:
| Category | CMS Language | Aligned Proposals |
| Chronic disease management and prevention | Promoting evidence-based, measurable interventions to improve prevention and chronic disease management. | eClinicalWorks (Proposals 3 and 4), Nest Health, Health Recovery Solutions, VSee |
| Payment Systems | Providing payments to health care providers for the provision of health care items or services, as specified by the Administrator. | Hopscotch Primary Care |
| Tech solutions: chronic diseases and prevention | Promoting consumer-facing, technology-driven solutions for the prevention and management of chronic diseases. | Build Cities, eClinicalWorks (Proposals 3, 4, and 7), Health Recovery Solutions, Syntasa (Proposals 1 and 3), White-Label Telehealth Solutions, RadleyCare, VSee |
| Tech solutions: remote monitoring, AI, etc. | Providing training and technical assistance for the development and adoption of technology-enabled solutions that improve care delivery in rural hospitals, including remote monitoring, robotics, artificial intelligence, and other advanced technologies. | AngelEye Health, eClinicalWorks (Proposal 6), Harbor, Health Recovery Solutions, Hopscotch Primary Care, OnMed, Syntasa (Proposal 2), White-Label Telehealth Solutions, RadleyCare, VSee |
| Retaining rural workforces | Recruiting and retaining clinical workforce talent to rural areas, with commitments to serve rural communities for a minimum of 5 years. | Google Cloud (Proposal 2), Hopscotch Primary Care, RadleyCare |
| Software infrastructure and technology | Providing technical assistance, software, and hardware for significant information technology advances designed to improve efficiency, enhance cybersecurity capability development, and improve patient health outcomes. | eClinicalWorks (Proposals 1, 5, and 7), Google Cloud (Proposals 1 and 3), OnMed, RadleyCare, VSee |
| Right-size delivery systems | Assisting rural communities to right-size their health care delivery systems by identifying needed preventative, ambulatory, pre-hospital, emergency, acute inpatient care, outpatient care, and post-acute care service lines. | AngelEye Health, eClinicalWorks (Proposal 5), Nest Health |
| Behavioral health | Supporting access to opioid use disorder treatment services (as defined in section 1861(jjj)(1)), other substance use disorder treatment services, and mental health services. | Build Cities, Syntasa (Proposal 2), RadleyCare |
| Value-based care | Developing projects that support innovative models of care that include value-based care arrangements and alternative payment models, as appropriate. | eClinicalWorks (Proposal 2), Hopscotch Primary Care, Nest Health |
Appendix
AngelEye Health, Inc.
Summary: Digital Health Solutions for Rural Families with Medically Complex Children
Contact: David Landman, Chief Commercial Officer, [email protected]
Executive Summary
AngelEye Health is a digital health company dedicated to improving complex pediatric outcomes through technology-enabled family engagement, feeding management, and care coordination. With current solutions already deployed across hundreds of the nation’s NICUs, AngelEye is uniquely positioned to extend these benefits to rural hospitals and families. Our platform strengthens caregiver confidence, helps manage length of stay, and improves neonatal outcomes—all priorities of the Rural Health Transformation Program (RHTP).
By empowering rural hospitals to leverage these proven tools, AngelEye helps bridge geographic and socioeconomic gaps in neonatal care, enabling families to remain engaged in their child’s care even when distance, work, or caregiving responsibilities limit in-person presence.
AngelEye Solutions for Rural Health
Solution 1: AngelEye Camera System: Connecting Families Across Distance
- Challenge: Parents in rural communities often live hours from the NICU, creating barriers to bonding and involvement.
- Solution: Secure, HIPAA-compliant video streaming allows parents and caregivers to remain virtually present with their hospitalized child.
Impact:
- Strengthens family engagement and bonding, which research links to improved health outcomes.
- Reduces caregiver stress and absenteeism while enabling ongoing family support.
- Improve patient & family satisfaction by maintaining family involvement and confidence in care planning.
Solution 2: AngelEye MilkTracker: End-to-End Milk Scanning & Feeding Management
- Challenge: Accurate feeding management is critical for neonatal outcomes, yet rural NICUs often lack advanced digital tools.
- Solution: End-to-end digital feeding management system ensuring precision in handling, labeling, and administration of breastmilk and formula.
Impact:
- Reduces feeding errors and improves clinical efficiency.
- Enhances long-term outcomes for medically fragile neonates.
- Helps rural hospitals lower costs associated with complications and re-hospitalizations.
Solution 3: AngelEye NICU2Home: Evidence-Based NICU Navigation & Discharge Coordination
- Challenge: Rural families face knowledge gaps and logistical challenges in preparing for discharge.
- Solution: Daily personalized updates, dynamic education tailored to the baby’s age and condition, and discharge readiness tracking.
Impact:
- Improves caregiver confidence and competence.
- Reduces avoidable discharge delays and readmissions.
- Enhances nursing efficiency by automating educational tasks.
Alignment with Rural Health Transformation Program Goals
AngelEye’s integrated platform could advance RHTP priorities in multiple categories:
- Technology & Innovation: Bring proven digital tools to underserved rural hospitals, improving efficiency and outcomes.
- Family Engagement & Prevention: Strengthen caregiver involvement, which is linked to improved neonatal development and reduced complications.
- Workforce Support: Improve nursing efficiency, allowing rural hospitals to better manage staff shortages.
- Cost Efficiency: Reduce length of stay, feeding errors, and readmissions, lowering financial strain on hospitals and payers.
Why This Matters for Rural Health Transformation:
- NICU-level care is both common (roughly 10% of all US births) and cost-intensive, especially for medically complex neonates—many of whom are served under Medicaid.
- Rural hospitals, which often operate on narrow margins, stand to benefit significantly from interventions that can reduce NICU length of stay, minimize errors, and enhance caregiver readiness—thus lowering downstream healthcare costs and improving outcomes.
Future Innovation & Sustainability
All solutions are built on a unified platform, ensuring seamless integration for hospitals, families, and care teams. Importantly, these tools are scalable, sustainable, and already proven in diverse hospital settings across the country.
AngelEye’s solutions could lay the foundation for future innovations currently in R&D, such as camera-based algorithms or virtual rounding to further support clinical teams in remote and resource-limited settings.
Organizational Background
AngelEye Health has over a decade of experience in neonatal digital health solutions and currently serves hundreds of NICUs nationwide. Our expertise lies in developing evidence-based tools that combine technology, family engagement, and clinical efficiency to improve complex pediatric outcomes.
Conclusion
By equipping rural hospitals with AngelEye’s proven digital health solutions, the RHTP can directly improve outcomes for medically complex neonates, strengthen caregiver confidence, and reduce systemic costs. AngelEye Health is ready to partner with states and rural health providers to implement these scalable, evidence-based solutions, ensuring that geography is no longer a barrier to family-centered neonatal care.
More information: www.angeleyehealth.com/solutions
Build Cities
Contact: Nick Smoot, CEO, 208-818-0654
Executive Summary
Build Cities is a community contribution platform that serves as the social, civic, and economic operating system for communities. The platform provides a single system that every community in a state can use to meet local needs while also producing consistent contribution data.
At its core, Build Cities:
- Verifies community contribution hours for volunteering, workforce training, and innovation projects, directly supporting Medicaid workforce requirements.
- Connects residents to healthcare institutions and to one another through challenges, projects, and events that reduce isolation and build belonging.
- Delivers prevention and chronic disease solutions by making community-led efforts to address health-related challenges trackable and rewarding.
- Routes residents to workforce-relevant opportunities that strengthen recruitment, retention, and training pipelines in rural areas.
- Captures data and feedback on quality of life, belonging, and engagement, which flows back to hospitals, providers, and state leaders.
Build Cities reframes compliance as contribution and transforms rural healthcare into a system that combines purpose, prevention, and participation.
Alignment with RHTP Categories
1. Improve Access to Hospitals, Providers, and Services
Residents can be connected directly to local stakeholder institutions such as clinics and hospitals, which can post challenges and projects for patients, employees, and community members to solve. This builds a community around hospitals and clinics where residents collaborate on prevention initiatives, chronic disease management, and local healthcare needs. Data on participation and engagement flows directly to stakeholders, strengthening access and coordination.
2. Improve Healthcare Outcomes for Rural Residents
Healthcare outcomes improve when people have purpose, belonging, and support networks. Build Cities enables rural residents to participate in projects that matter to them, creating social capital and attitudes of personal ownership toward solving local challenges including prevention and care. By turning residents into contributors, the platform fosters healthier behaviors, reduces depression and isolation, and strengthens continuity of care.
3. Prioritize New and Emerging Technologies for Prevention and Chronic Disease Management
Build Cities uses AI-driven coaching and project matching to engage residents in prevention-focused activities. Nutrition initiatives, walking clubs, and peer support networks are examples. Participants earn time credits, points, and recognition for their contributions. In some cases, community-led solutions to chronic disease prevention could attract funding or philanthropic support to scale innovations.
4. Enhance Economic Opportunity and Clinician Supply through Recruitment and Training
The platform provides pathways to workforce opportunity by connecting residents to in-demand skills training, volunteering, and innovation challenges that can lead to new companies being funded and formed. By deepening ties between families, communities, and local healthcare providers, Build Cities strengthens retention and helps rural areas recruit and keep clinicians. The social infrastructure created by Build improves economic stability and makes rural communities more attractive places to live and work.
5. Prioritize Data and Technology-Driven Solutions Close to Home
Build Cities captures real-time data on community connections, belonging, and participation. This data helps rural hospitals and providers understand how patients are engaging in prevention, community life, and workforce development. By delivering insights close to home, Build supports high-quality care, better patient engagement, and proactive solutions to community needs. It also serves as a way to collect data that can count toward Medicaid workforce and volunteer hours compliance.
General Plan for Implementation
Phase 1 – Foundation (Q1 2026):
- State agencies and providers define rural health priorities such as diabetes, maternal care, and behavioral health.
- Verified and approved challenges are pre-loaded into the platform.
Phase 2 – Community Onboarding (Q2 2026):
- Residents onboard app, SMS, or at community hub activation events such as clinics, cooperative extensions, or churches.
- AI routes residents to projects based on skills, goals, and health needs.
Phase 3 – Verification and Feedback (Q3 2026):
- Hours verified through AI milestones, patient digital journals and feedback, or challenge sponsor validation.
- NPS-style patient and resident feedback captured via digital tools and at events.
- Community contribution data aggregated into dashboards for progress and compliance reporting.
Phase 4 – Scale and Network (Q4 2026 and beyond):
- Expand the platform to more rural communities as one shared system for compliance, belonging, and innovation.
- Blend state, philanthropic, and private sector funding to increase engagement on challenges and financial support for projects.
- Share best practices for community engagement and health across the statewide network.
Why It Matters
- Compliance with Dignity: Keeps rural residents on Medicaid by providing verifiable hours for volunteering, skills training, and innovation.
- Belonging and Purpose: Builds social infrastructure that reduces loneliness and depression by connecting neighbors through contribution.
- Prevention and Chronic Disease: Incentivizes residents to engage in prevention projects and health challenges.
- Workforce Pathways: Strengthens recruitment, retention, and training pipelines by aligning participation with in-demand skills.
- Data for Clinics and Hospitals: Provides real-time data and feedback on patient engagement, quality of life, and community needs.
- One System Statewide: Creates a unified operating system used in every rural community, tailored to local needs and connected across the state.
Conclusion
Rural healthcare transformation requires more than financial stabilization and more providers. It requires a new operating system for communities that integrates compliance, prevention, belonging, and connection into everyday life.
Build Cities can provide that system:
- A community contribution platform that verifies hours for Medicaid requirements.
- A civic and social infrastructure that reduces isolation and creates purpose.
- A data engine that informs hospitals and state leaders in real time.
- A single system every rural community can use to meet its local needs while contributing to statewide goals.
By reframing compliance as contribution, Build Cities ensures rural residents stay covered, stay connected, and stay hopeful while hospitals, providers, and states gain the data and infrastructure they need to thrive.
eClinicalWorks, LLC
Contact: Vivek Mehta, Vice President, Health Centers, eClinicalWorks – [email protected], [email protected]
Proposal 1: Electronic Health Records
Executive Summary
eClinicalWorks® (eCW), together with its consumer-facing platform, healow®, offers a comprehensive, sustainable, and affordable technology ecosystem specifically designed to improve access to hospitals, healthcare providers, and essential healthcare services for rural residents. Through a unified, cloud-based platform, eCW integrates ambulatory, inpatient, specialty, and virtual care, enabling rural health organizations to optimize patient access, continuity, and outcomes.
Unified EHR Platform Designed for Rural Needs
The ONC-certified eClinicalWorks V12 platform delivers a single, integrated electronic health record for ambulatory care, practice management, and soon, Critical Access Hospital (CAH) inpatient workflows (live in 2026). This system includes modules for Behavioral Health (inpatient and outpatient), Ambulatory Surgery Center (ASC), Emergency Room (ER), and a fully integrated pharmacy solution (available Q4 2025).
- “One Patient, One Chart”: Patients benefit from a unified record across clinics, hospitals, ERs, behavioral health, dental, vision, and pharmacy. This seamless integration ensures vital information follows the patient, improving continuity, coordination, and safety—key to rural access where care occurs across multiple, often dispersed sites.
Direct Solutions to Rural Access Barriers
eCW and healow® connect patients to care in new, patient-centered ways:
healow Open Access
- Enables new and returning patients to find providers (by time, specialty, or location) online, book or request appointments, receive confirmations, and reminders—all without requiring a phone call or in-person visit.
- This solution is critical in areas with provider shortages, transportation challenges, or limited office hours, breaking down common rural access barriers.
Telehealth and healow TeleVisits™
- Fully integrated telemedicine enables safe, convenient virtual care on any device—computer, smartphone, or tablet—with direct documentation into the core EHR.
- Features include virtual waiting rooms, screen sharing, group telehealth sessions, and eClinicalTouch® for on-the-go care delivery.
healow Mobile Health Apps
- Patient-facing mobile apps (iOS and Android) deliver all Patient Portal features—messaging, test results, appointment scheduling, prescription requests, and provider communications—anytime, anywhere.
healow CHECK-IN™
- Contactless, smartphone-enabled solution lets patients check in remotely, complete forms, update demographics/insurance, and pay bills or copays. This reduces wait times, streamlines workflows, and makes care more accessible for rural residents.
healow Meet
- Providers can host and manage group audio or telehealth visits—ideal for shared education, behavioral health counseling, and chronic condition management.
Addressing Every Rural Setting
eClinicalWorks supports a diversity of rural organizations by providing targeted modules for:
- Rural Health Clinics (RHCs), Federally Qualified Health Centers (FQHCs), Tribal Health, and Community Health
- Ambulatory Surgical Centers (ASC) and Emergency Services/ER
- Behavioral Health, including inpatient residential environments
- Pharmacy (340B integration and in-house dispensing)
- Critical Access Hospitals (CAH) EHR, launching in 2026
All modules interact seamlessly, allowing even smaller clinics or critical access hospitals to offer full-spectrum, patient-centered care.
Proven Results and Real-World Impact
eClinicalWorks has a deep history of partnering with community-based health organizations to reduce disparities and improve access. A signature example is its selection as the sole EHR vendor for New York City’s Primary Care Information Project (PCIP)—one of the nation’s largest community-based EHR implementations (750+ facilities, 3,000+ providers). Working with the NYC Department of Health, eCW enabled real-time clinical decision support and point-of-care alerts, resulting in measurable improvements in quality and access, including:
- Increases in cancer screening, diabetes control, hypertension management, and smoking cessation counseling
- Consistent data and care across thousands of providers, benefiting millions of residents
These demonstrated, peer-reviewed results are directly translatable to rural health settings, where eClinicalWorks now serves over 800 RHCs, FQHCs, CHCs, and Tribal Health organizations nationwide.
Affordable, Scalable, and Rural-Ready
- Cloud Deployment & Affordable Pricing:
- Minimal hardware and IT staffing needs allow rural providers to adopt enterprise-grade solutions at lower costs and with reduced operational burdens.
- Continuous Product Innovation:
- Rapid updates and feature enhancements, including integrated artificial intelligence, allow organizations to streamline workflows and automate routine tasks—improving provider capacity and reducing burnout.
Responding to Patient and Provider Needs
Over years of real-world experience—including responses to the COVID-19 pandemic—eClinicalWorks and healow® have developed tools that put patient, provider, and staff access and safety at the forefront. Features such as contactless check-in, remote registration, and AI-driven task automation help rural health organizations address both new and longstanding access barriers, ensuring every patient has a convenient, safe path to care.
Summary and Commitment
eClinicalWorks® and healow® directly advance the aims of Category 1 by making it possible for rural residents to discover, book, and receive the full range of care—ambulatory, inpatient, specialty, and telehealth—at the right place and time, with streamlined communication and continuity. This technology ecosystem, validated in large-scale public health deployments and shaped by the real-world needs of rural providers and patients, is uniquely equipped to transform access, reduce disparities, and drive measurable improvements in rural health.
Proposal 2: Value-Based Care
eClinicalWorks® (eCW) is dedicated to improving health outcomes for rural populations by providing healthcare organizations with integrated, evidence-based technology solutions. Through the deployment of our EHR platform, practice-proven care management modules, and advanced data analytics, eClinicalWorks empowers rural providers to achieve measurable improvements in chronic disease management, prevention, and holistic patient care.
Documented Impact—Evidence from New York City PCIP
eCW’s effectiveness is demonstrated by our partnership with the New York City Primary Care Information Project (PCIP)—one of the nation’s largest community-based EHR deployments. Multiple studies and real-world outcomes have documented substantial improvements in clinical quality and health outcomes for over four million New Yorkers, a model directly applicable to rural health settings:
- Diabetes: Among 81,000 patients, the percentage receiving routine hemoglobin A1c tests improved from 46% to 58%, resulting in greater diabetes management and control.
- Hypertension: 96,000 patients improved their blood pressure control; the percentage of patients reducing dangerously high systolic readings by 20mmHg or more increased from 55% to 64%.
- Smoking Cessation: 58,000 smokers engaged in counseling or medication to quit, with intervention rates rising from 29% to 46%. This contributed to New York City achieving the lowest rate of smoking-related deaths nationwide.
eClinicalWorks’ collaboration across hundreds of sites and thousands of providers enabled rapid adoption of evidence-based clinical quality measures, clinical pathway best practices, and patient engagement strategies—driving measurable improvements in outcomes that can be replicated in rural settings nationwide.
Patient Engagement & Value-Based Care for Better Outcomes
Building on PCIP and nationwide experience with community health organizations, eCW deploys integrated, outcome-focused modules designed to address every step of the patient journey:
- Ambulatory EHR & Patient Engagement: Engages patients with reminders, education, and seamless communication—empowering them to participate in their care, close gaps, and complete essential screenings.
- Value-Based Care (VBC) Suite: Supports practices participating in CMS quality incentive programs (MIPS, HEDIS, PCMH, etc.) and offers tools purpose-built for the prevention and management of chronic conditions:
- Chronic Care Management (CCM)/Principal Care Management (PCM): Enables tracking and reimbursement for care coordination activities, helping ensure that patients receive regular follow-up and support between visits.
- Remote Patient Monitoring (RPM): Connects home monitoring devices with the EHR, allowing providers to track vital signs and disease management remotely and intervene earlier to reduce hospitalizations.
- Care Plan Oversight (CPO): Structures and tracks provider time for patients with complex medical needs, ensuring high-touch, compliant care management.
- Transition Care Management (TCM): Enhances communication and follow-up when patients move between hospitals, clinics, and home, reducing readmissions and preventable complications
- Disease Explorer and Population Health: Practices can stratify patient populations, group at-risk cohorts, and dynamically identify opportunities to close gaps in screening, prevention, and disease management.
- Hierarchical Condition Coding (HCC): Promotes accurate risk assessment and prediction of healthcare needs, enabling more personalized, risk-adjusted management for rural populations.
Leveraging Artificial Intelligence for Rural Health Outcomes
eClinicalWorks embeds artificial intelligence (AI) across modules to help rural providers and care teams proactively address gaps and optimize care:
- CIPHR (Clinical Intelligence for Population Health Record):
- A real-time population health analytics dashboard that displays active cohorts, tracks clinical quality measures, reveals care gaps, and enables drilldown for actionable intervention at the patient and population level.
- No Show Predictor:
- AI/ML tools predict with 90% accuracy which appointments are likely to be missed or canceled. This enables practices to deploy outreach strategies, double-book when needed, and keep patients engaged and schedules full, a key for populations facing barriers like transportation or work conflicts.
- Holistic, Patient-Centered View:
- eCW AI and clinical intelligence modules unify data streams (screenings, HEDIS/MIPS/QI, remote monitoring, SDOH, and more), informing clinical decisions and allowing truly whole-person care for rural patients who may see multiple providers.
Population Health and Preventive Care
- Proactive Screening and Early Detection:
- eCW enables practices to use real-time data and decision support to identify care gaps, manage preventive alerts, and deliver prompts for vital screenings (cancer, diabetes, cardiovascular, vaccinations).
- Chronic Disease Management:
- Automated reminders and monitoring tools help ensure that high-risk patients maintain disease control, reducing avoidable ED visits and hospitalizations, and supporting healthier long-term outcomes.
Outcomes and Financial Incentives
eClinicalWorks supports organizations as they shift to value-based models, providing transparency and support for regulatory and payer initiatives. Practices using eCW are positioned to:
- Earn incentives and avoid penalties in CMS programs by easily and accurately reporting outcomes and compliance.
- Demonstrate measurable improvements in chronic and preventive care, directly supporting Rural Health Transformation Program goals.
Conclusion
Through real-world validated technology, proven care management modules, and innovative AI, eClinicalWorks delivers the tools rural organizations need to drive better outcomes, reduce disparities, and provide population health management for every resident. The eClinicalWorks solution enables rural organizations to engage patients, leverage data, and close care gaps—ensuring lasting health improvements at both the individual and community levels.
eClinicalWorks stands ready to support the state’s Rural Health Transformation Program by delivering measurable enhancements to population health outcomes in rural communities.
Proposal 3: Primary Care Information
Executive Summary
eClinicalWorks® (eCW) is dedicated to improving health outcomes for rural populations by providing healthcare organizations with integrated, evidence-based technology solutions. Through the deployment of our EHR platform, practice-proven care management modules, and advanced data analytics, eClinicalWorks empowers rural providers to achieve measurable improvements in chronic disease management, prevention, and holistic patient care.
Documented Impact—Evidence from New York City PCIP
eCW’s effectiveness is demonstrated by our partnership with the New York City Primary Care Information Project (PCIP)—one of the nation’s largest community-based EHR deployments. Multiple studies and real-world outcomes have documented substantial improvements in clinical quality and health outcomes for over four million New Yorkers, a model directly applicable to rural health settings:
- Diabetes: Among 81,000 patients, the percentage receiving routine hemoglobin A1c tests improved from 46% to 58%, resulting in greater diabetes management and control.
- Hypertension: 96,000 patients improved their blood pressure control; the percentage of patients reducing dangerously high systolic readings by 20mmHg or more increased from 55% to 64%.
- Smoking Cessation: 58,000 smokers engaged in counseling or medication to quit, with intervention rates rising from 29% to 46%. This contributed to New York City achieving the lowest rate of smoking-related deaths nationwide.
eClinicalWorks’ collaboration across hundreds of sites and thousands of providers enabled rapid adoption of evidence-based clinical quality measures, clinical pathway best practices, and patient engagement strategies—driving measurable improvements in outcomes that can be replicated in rural settings nationwide.
Patient Engagement & Value-Based Care for Better Outcomes
Building on PCIP and nationwide experience with community health organizations, eCW deploys integrated, outcome-focused modules designed to address every step of the patient journey:
- Ambulatory EHR & Patient Engagement: Engages patients with reminders, education, and seamless communication—empowering them to participate in their care, close gaps, and complete essential screenings.
- Value-Based Care (VBC) Suite: Supports practices participating in CMS quality incentive programs (MIPS, HEDIS, PCMH, etc.) and offers tools purpose-built for the prevention and management of chronic conditions:
- Chronic Care Management (CCM)/Principal Care Management (PCM): Enables tracking and reimbursement for care coordination activities, helping ensure that patients receive regular follow-up and support between visits.
- Remote Patient Monitoring (RPM): Connects home monitoring devices with the EHR, allowing providers to track vital signs and disease management remotely and intervene earlier to reduce hospitalizations.
- Care Plan Oversight (CPO): Structures and tracks provider time for patients with complex medical needs, ensuring high-touch, compliant care management.
- Transition Care Management (TCM): Enhances communication and follow-up when patients move between hospitals, clinics, and home, reducing readmissions and preventable complications.
- Disease Explorer and Population Health: Practices can stratify patient populations, group at-risk cohorts, and dynamically identify opportunities to close gaps in screening, prevention, and disease management.
- Hierarchical Condition Coding (HCC): Promotes accurate risk assessment and prediction of healthcare needs, enabling more personalized, risk-adjusted management for rural populations.
Leveraging Artificial Intelligence for Rural Health Outcomes
eClinicalWorks embeds artificial intelligence (AI) across modules to help rural providers and care teams proactively address gaps and optimize care:
- CIPHR (Clinical Intelligence for Population Health Record):
- A real-time population health analytics dashboard that displays active cohorts, tracks clinical quality measures, reveals care gaps, and enables drilldown for actionable intervention at the patient and population level.
- No Show Predictor:
- AI/ML tools predict with 90% accuracy which appointments are likely to be missed or canceled. This enables practices to deploy outreach strategies, double-book when needed, and keep patients engaged and schedules full, a key for populations facing barriers like transportation or work conflicts.
- Holistic, Patient-Centered View:
- eCW AI and clinical intelligence modules unify data streams (screenings, HEDIS/MIPS/QI, remote monitoring, SDOH, and more), informing clinical decisions and allowing truly whole-person care for rural patients who may see multiple providers.
Population Health and Preventive Care
- Proactive Screening and Early Detection:
- eCW enables practices to use real-time data and decision support to identify care gaps, manage preventive alerts, and deliver prompts for vital screenings (cancer, diabetes, cardiovascular, vaccinations).
- Chronic Disease Management:
- Automated reminders and monitoring tools help ensure that high-risk patients maintain disease control, reducing avoidable ED visits and hospitalizations, and supporting healthier long-term outcomes.
Outcomes and Financial Incentives
eClinicalWorks supports organizations as they shift to value-based models, providing transparency and support for regulatory and payer initiatives. Practices using eCW are positioned to:
- Earn incentives and avoid penalties in CMS programs by easily and accurately reporting outcomes and compliance.
- Demonstrate measurable improvements in chronic and preventive care, directly supporting Rural Health Transformation Program goals.
Conclusion
Through real-world validated technology, proven care management modules, and innovative AI, eClinicalWorks delivers the tools rural organizations need to drive better outcomes, reduce disparities, and provide population health management for every resident. The eClinicalWorks solution enables rural organizations to engage patients, leverage data, and close care gaps—ensuring lasting health improvements at both the individual and community levels.
eClinicalWorks stands ready to support the state’s Rural Health Transformation Program by delivering measurable enhancements to population health outcomes in rural communities.
Proposal 4: Chronic Disease Management
Executive Summary
eClinicalWorks® (eCW) provides a comprehensive, technology-driven suite of solutions empowering rural health organizations to leverage innovation for the prevention and management of chronic diseases. The Company’s offerings—including value-based care modules, unified analytics, population health reporting, and integrated clinical decision support—drive measurable improvements in chronic disease outcomes, reduce costs, and streamline compliance for providers and health centers.
Comprehensive Technology Ecosystem for Chronic Disease Management
Value-Based Care Suite
- Chronic Care Management (CCM) & Principal Care Management (PCM):
- Supports providers in delivering non-face-to-face care coordination for patients with multiple or single chronic conditions and automates documentation for CMS reimbursement. This ensures high-risk rural populations are proactively managed, even outside scheduled visits.
- Remote Patient Monitoring (RPM):
- The RPM module collects patient physiological data from connected devices, enabling providers to monitor vital health trends remotely, respond quickly to changes, and reduce unnecessary hospital admissions and acute episodes.
- Care Plan Oversight (CPO):
- CPO capabilities allow providers to track and document certified and recertified status for complex cases, measure clinical staff time, and ensure ongoing, high-touch care for rural patients.
- Transition Care Management (TCM):
- Ensures safe and efficient transitions for patients moving between hospitals, clinics, and home care by tracking appointments, reconciling medications, and supporting regulatory compliance. This reduces readmissions and improves patient safety in dispersed rural regions.
Population Health and Risk Analytics
- Disease Explorer:
- Enables practices to segment populations into cohorts, focus on high-risk patients, investigate disease risk, and close care gaps—empowering targeted outreach and effective resource allocation.
- Hierarchical Condition Category (HCC) Coding:
- Integrated HCC dashboards identify risk gaps, display Risk Adjustment Factor (RAF) scores, and allow for trending and year-over-year analysis. This supports value-based contracts and accurate forecasting for financial and care management.
- Patient-Centered Medical Home (PCMH) Model:
- Encourages primary care excellence and population health coordination; facilitates data-driven approaches to lowering costs and improving rural health outcomes through standardized, patient-centered pathways.
Regulatory Reporting and Quality Insights
- MIPS & HEDIS Measures:
- eCW automates the calculation and reporting for Merit-Based Incentive Payment System (MIPS) and Healthcare Effectiveness Data and Information Set (HEDIS), supporting performance measurement, population health planning, and regulatory compliance.
- Built-in Rural Health & Community Reporting:
- Unified reporting covers UDS (Uniform Data System), Medicare & Medicaid, 340B pharmacy, cost reports, HIV, Ryan White, Title X Family Planning, Dental (NNOHA), Tribal Health, and state-specific metrics. Practices can easily monitor performance, identify improvement areas, and demonstrate accountability.
Integrated Clinical Decision Support and Automation
- Clinical Decision Support System (CDSS):
- eCW provides real-time, protocol-driven reminders for disease management and prevention (screenings, labs, immunizations). These reminders are based on evidence and customized for individual patient profiles using demographic and clinical data.
- Clinical Rules Engine (CRE):
- Practices configure rules to automate preferred clinical pathways and set alert levels for critical values. Automated workflows ensure prompt action, timely follow-up, and adherence to preventive and chronic care protocols.
- Clinical Rules Engine (CRE):
- Practices can customize and schedule patient-facing alerts for disease management, preventive care, and wellness, helping address barriers to compliance often seen in rural settings.
Artificial Intelligence for Population Health and Adherence
- CIPHR (Clinical Intelligence for Population Health Record):
- This AI-powered, optional analytics dashboard gives teams a real-time, holistic view of active patient populations, tracks clinical quality measures, pinpoints care gaps, and allows intervention down to the individual patient. Data integration from HEDIS, MIPS, and additional sources ensures meaningful, actionable population health insights.
- AI-Based Compliance & No-Show Management:
- Machine learning predicts patient appointment no-shows and cancellations with over 90% accuracy, enabling practices to double-book, notify those on a waitlist, or open high-risk slots online. This technology maximizes clinical capacity and ensures critical chronic care visits are filled, which is particularly important in resource-limited rural environments.
Practice-Level Effectiveness and Rural Impact
eClinicalWorks empowers rural health centers and critical access hospitals to implement best practices, lower barriers, and deliver continuous improvement across chronic disease prevention and management:
- Optimize care for prevalent rural chronic conditions, such as diabetes, cardiovascular disease, COPD, and hypertension.
- Streamline regulatory compliance, reducing administrative burden while maximizing value-based payments and incentives.
- Provide holistic, longitudinal care—helping providers go beyond episodic treatment and offer proactive, sustained support.
Conclusion
eClinicalWorks equips rural health organizations with robust, integrated technologies to transform chronic disease management through prevention, monitoring, patient engagement, AI-driven analytics, and clinical automation. Our solutions deliver proven results in closing care gaps, improving patient outcomes, controlling costs, and enhancing the effectiveness of rural healthcare teams.
Proposal 5: Interoperable Technology
Executive Summary
eClinicalWorks® (eCW) is uniquely positioned to help rural hospitals and healthcare providers foster, strengthen, and sustain local and regional partnerships. By offering a unified, cloud-based platform that connects inpatient, outpatient, behavioral health, and specialty care across multiple organizations, eClinicalWorks enables collaborative care, cost efficiencies, and best practices.
Strengthening Regional Partnerships Through Interoperable Technology
Interoperability First
eClinicalWorks is a Qualified Health Information Network® (QHIN™) and active Carequality® participant, ensuring robust, secure, and seamless exchange of health information among rural hospitals, clinics, FQHCs, RHCs, behavioral health facilities, ASCs, and emergency departments. Real-time data exchange allows for coordinated referrals, shared care plans, and smooth transitions across organizations—helping to establish and maintain trust and efficiency within partnerships.
Unified Patient Record
eCW’s ambulatory and inpatient solutions ensure that all partners in a health network access the same “one patient, one chart” system. This continuity prevents fragmentation, guarantees everyone has the most up-to-date information, and allows best practices in care delivery to travel with the patient as they move through different providers within the region.
Ambulatory Surgical Center (ASC) Solution
Designed for efficiency, the eCW ASC module centralizes scheduling, documentation, and resource management. By standardizing these workflows, ASCs can partner seamlessly with hospitals and clinics, creating an integrated surgical care network. The built-in virtual assistant “Eva™” automates administrative tasks—supporting capacity and minimizing overhead system-wide.
Emergency Room Module
eClinicalWorks’ emergency room solution helps rural hospitals and urgent care centers operate as unified emergency networks. Real-time ER census, patient tracking, eMAR, and integrated documentation tools ensure that, regardless of a patient’s entry point, information flows securely among partner sites, supporting collaboration during high-acuity care and enabling resource sharing.
24 Hour Behavioral Health
The 24-hour behavioral health module bridges outpatient providers and residential behavioral health facilities. With shared registration, bed management, order entry, eMAR, and seamless flow of patient information, rural hospitals and behavioral health organizations can work as one integrated care team, optimizing bed utilization and improving continuity for vulnerable patients.
Future Products
The eClinicalWorks Pharmacy Module will be released in Q4 of 2025, and a Critical Access Hospital (CAH) inpatient EHR Solution will Go Live in 2026.
Driving Collective Quality Improvement and Cost Efficiencies
Centralized Reporting, Analytics, and Quality Dashboards
Across an enterprise using eClinicalWorks, all facilities can share a single database, allowing them to generate unified, enterprise-level reports for cost (cost reporting), quality (MIPS, HEDIS), and compliance. Population health and gap analysis dashboards enable collaborative tracking of initiatives, alignment on best practices, and peer benchmarking—the building blocks of region-wide quality improvement.
Economies of Scale
Cloud deployment means partner organizations save on IT infrastructure and support, minimizing the burden on each site. Partners can also leverage unified purchasing, shared professional services, and pooled training, helping each organization—regardless of size—achieve greater financial stability and access to innovation.
Automated Documentation and Benchmarking Tools
With direct integration of eBO and advanced analytics, partners can auto-generate required quality and cost reports, identify improvement opportunities, and track benchmarks together. This eliminates redundant data entry, reduces manual errors, and ensures that smaller providers keep pace with the latest standards.
Practice Standardization and Best Practice Sharing
Through eCW’s customizable templates and treatment plans, healthcare systems can quickly implement evidence-based protocols at every site. Shared updates allow every provider to benefit from network-wide learning and innovation, regardless of their individual resources.
A Model of Collaborative Care in Action
Using eClinicalWorks, a rural regional health system connects its hospital, local clinics, ASCs, and behavioral health facilities on a single technology platform. Patient records, referrals, and treatment plans travel with the patient throughout the network—minimizing duplication and gaps in care. The group utilizes shared analytics dashboards for MIPS and HEDIS, runs collective quality initiatives, and shares best practices system-wide.
Conclusion
eClinicalWorks provides the foundation that rural health organizations need to create, operate, and optimize strong partnerships. By enabling real-time information exchange, collective quality measurement, and shared administration, eClinicalWorks maximizes economies of scale and accelerates the adoption of best practices throughout the region. Our platform helps rural hospitals and their partners promote measurable quality improvement, improve financial sustainability, and deliver more coordinated care to every rural resident.
eClinicalWorks stands ready to support the state in building resilient, high-performing rural networks that achieve measurable results and ensure access to quality healthcare for all.
Proposal 6: AI
Executive Summary
eClinicalWorks AI Bundle (Sunoh.AI, PRISMA, healow Genie)
eClinicalWorks offers an AI Bundle designed to transform rural health care delivery by improving efficiency, enhancing clinical decision-making, and expanding patient engagement. This bundle integrates three core innovations—Sunoh.AI, PRISMA, and healow Genie—to support providers and patients across the continuum of care.
Sunoh.AI – Ambient Listening and Documentation
Sunoh.AI is an AI-powered ambient listening tool that securely captures the natural patient–provider conversation and generates accurate, structured clinical documentation directly into the eClinicalWorks EHR. By reducing the time spent on manual charting, Sunoh.AI allows providers in rural hospitals and health centers to focus on direct patient care. This leads to improved efficiency, decreased provider burnout, and more comprehensive documentation for billing and compliance.
PRISMA – Nationwide Interoperability
PRISMA is an interoperability platform that consolidates patient records from hospitals, health systems, and the Carequality national interoperability network. PRISMA creates a longitudinal, timeline-based patient record accessible within the eClinicalWorks EHR. For rural providers who often face fragmented health information, PRISMA ensures they have the full clinical picture to guide evidence-based interventions, reduce duplication of services, and improve care coordination for patients with chronic and complex conditions.
healow Genie – AI-Powered Contact Center
healow Genie is an AI-driven virtual assistant that enhances patient engagement through natural, conversational interactions. It supports appointment scheduling, medication reminders, lab result access, and care management outreach, all available 24/7. By automating routine tasks and enabling patient self-service, healow Genie improves patient access, reduces no-show rates, and empowers rural patients to stay engaged with their care teams.
Impact on Rural Health Transformation
Together, the AI Bundle creates a synergistic solution:
- Efficiency Gains – Sunoh.AI reduces documentation burden, freeing up provider time.
- Better Decisions – PRISMA ensures rural providers access complete, interoperable patient data.
- Patient Engagement – healow Genie delivers scalable, consumer-facing engagement to bridge gaps in care.
By deploying this AI Bundle, eClinicalWorks enables rural health organizations to deliver higher-quality care, improve patient outcomes, and sustain long-term operational efficiency—directly aligning with the goals of the Rural Health Transformation Fund.
Promoting evidence-based, measurable interventions to improve prevention and chronic disease management
eClinicalWorks offers a comprehensive Population Health Management suite that supports evidence-based, measurable interventions to improve chronic disease prevention and management in rural communities.
The Remote Patient Monitoring (RPM) solution enables providers to track patient physiologic data such as blood pressure, glucose levels, and weight in real time. This data is integrated into the eClinicalWorks EHR, giving care teams actionable insights and alerts for early interventions.
Additionally, the Population Health bundle includes Chronic Care Management (CCM), Transition Care Management (TCM), and HEDIS Analytics, ensuring patients are managed under standardized care plans and that providers can close gaps in care. AI-powered outreach agents proactively engage patients with chronic conditions to ensure medication adherence, schedule follow-ups, and provide timely health education.
By enabling real-time engagement through telehealth and behavioral health tools, Rural Health Centers can intervene proactively, reducing hospitalizations and improving quality outcomes. These solutions are licensed under the Population Health bundle, allowing measurable improvements in chronic care outcomes and alignment with value-based care requirements.
Promoting consumer-facing, technology-driven solutions for the prevention and management of chronic diseases, healow, the consumer-facing platform from eClinicalWorks, provides rural patients with direct, technology-driven tools to manage and prevent chronic conditions. The healow app and portal—ranked highly on Apple and Android app stores—empower patients to engage with their providers, track vital health information, and receive personalized health guidance.
Through device connectivity, patients can share results from home monitoring devices such as blood pressure cuffs or glucometers directly with their care team, ensuring real-time feedback on their progress. The app also provides telehealth access to medical, dental, behavioral health, and vision services, enabling holistic care across multiple specialties.
healow’s features promote medication adherence, lifestyle management (diet, exercise, and mental health), and preventive care reminders. AI-enabled outreach further engages patients by sending reminders, educational resources, and personalized care recommendations. By leveraging these consumer-centric solutions, healow supports rural residents in taking active roles in their health, leading to better outcomes in the prevention and management of chronic diseases.
Providing training and technical assistance for the development and adoption of technology-enabled solutions that improve care delivery in rural hospitals
eClinicalWorks has a dedicated Training and Technical Assistance (TTA) program that equips rural hospitals and health centers with the knowledge and tools needed to successfully adopt advanced, technology-enabled solutions. Our training team provides hands-on and virtual instruction to providers, clinical staff, and administrators on the deployment of remote monitoring, AI tools, robotics integrations, and telehealth technologies.
Training includes modules on ambient listening (Sunoh.ai), AI-powered documentation and contact center solutions, language translation, voice-based patient engagement, and data analytics for care improvement. Beyond training, our team supports workflow redesign, change management, and ongoing optimization to ensure rural providers maximize efficiency and improve patient outcomes.
Conclusion
eClinicalWorks also provides technical assistance for cybersecurity readiness, interoperability deployment (via PRISMA), and the integration of AI-driven predictive models such as no-show prediction and medication adherence monitoring. These efforts enable rural providers to not only adopt but sustain the use of cutting-edge tools, resulting in reduced administrative burden, improved patient engagement, and measurable improvements in chronic care delivery.
Proposal 7: Universal Interoperability
Executive Summary
eClinicalWorks®: Interoperable, Secure, and Reliable Technology for Rural Healthcare
Transitioning rural healthcare from paper to electronic environments requires technology that is not only robust and affordable but also secure, reliable, interoperable, and user-friendly. eClinicalWorks® (eCW) provides a future-ready platform that connects hospitals, Rural Health Centers (RHCs), Critical Access Hospitals (CAHs), specialty providers, and patients—powering the seamless exchange of health data within and beyond rural communities.
Universal Interoperability at the Core
eClinicalWorks® leads in national and local interoperability, enabling rural providers to securely and efficiently exchange clinical data with any EHR, health information exchange, specialty practice, or hospital, regardless of geography or vendor.
- Carequality® Framework:
- As a founding member, eCW drives the public-private approach to seamless data exchange nationwide. This framework standardizes technical specifications, legal agreements, and directories, providing the backbone of interoperability for rural health organizations.
- Qualified Health Information Network® (QHIN™):
- eCW’s 2025 QHIN™ designation positions it among the first vendors enabling exchange through the Trusted Exchange Framework and Common Agreement™ (TEFCA™).
- PRISMANet: eCW’s QHIN ensures providers have the most complete patient information at the point of care, improving outcomes and closing information gaps for remote and rural patients.
- Direct Messaging & HISP certification:
- eCW supports secure, standards-based messaging between all providers, even on different EHRs, and is certified as a Health Information Service Provider (HISP).
State-of-the-Art Interoperability Tools
- PRISMA Health Information Search Engine:
- Offers providers a unified, real-time view of a patient’s history from internal and external sources—including other EHRs via the Carequality network, payer data, wearable devices, and patient questionnaires—organized into a searchable timeline.
- This holistic view is critical for ensuring the most informed care in rural environments, where patients may receive care in multiple settings.
- Peer-to-Peer (P2P®) Communication:
- Secure, direct exchange of summaries, problem lists, labs, imaging, and documents among trusted providers—simplifying coordination and encouraging care team collaboration.
- 360X Project Participation (ONC):
- Improves referrals and care transitions by automating bidirectional data flow between referring providers and specialists, closing referral loops, and ensuring no information is lost—especially important for rural residents who may need access to expertise not locally available.
National Digital Health Standards and Integrations
- HL7 and FHIR APIs:
- eCW supports uni- and bidirectional HL7 interfaces for lab and imaging and exposes Fast Healthcare Interoperability Resources (FHIR®) APIs for universal compatibility.
- Third-party developers and vendors can connect apps for both patient- and provider-facing workflows, expanding care delivery options and digital innovation in rural healthcare.
- SMART on FHIR capabilities enable plug-and-play applications directly with the eCW EHR/PM platform, with both read and soon-to-be-available write-back functionality.
- eCW supports uni- and bidirectional HL7 interfaces for lab and imaging and exposes Fast Healthcare Interoperability Resources (FHIR®) APIs for universal compatibility.
- App Gallery & Open Integration:
- An extensive ecosystem of third-party apps and integrations (see: eClinicalWorks FHIR App Gallery eCW’s FHIR Developer Platform allows health organizations to quickly add new tools tailored to their needs.
- Health Information Exchange (HIE) Connectivity:
- Upon request, eCW connects securely to regional, state, or national HIEs, supporting bi-directional flow, data enrichment, and robust care coordination.
Reliability, Security, and Accessibility
- Web-Based, Cloud-Hosted Platform:
- Hosted on Microsoft Azure, eCW delivers always-on, scalable, and secure access for providers and patients, especially as rural broadband expands. Accessed via modern browsers, it ensures minimal IT overhead and high reliability for every rural organization.
- Industry-Leading Security:
- eCW employs comprehensive security features—data encryption, secure messaging, access auditing, and redundancy—to protect sensitive patient data and meet stringent federal and state standards.
Empowering Patient Engagement and Virtual Access
- healow® TeleVisits and Mobile Apps:
- eCW’s patient-facing technologies bridge physical barriers by enabling secure telehealth visits and mobile messaging—even in challenging rural terrain or during inclement weather.
- healow App:
- Offers patients intuitive, on-demand access to appointments, medication requests, test results, secure messages, and provider communication—all via smartphone. This enhances rural patient engagement while supporting secure, electronic care.
Built for the Evolving Rural Landscape
eCW’s flexibility and cloud-based design ensure that as federal and state programs expand rural connectivity, organizations can rapidly adopt robust EHRs and patient-facing tools with a low total cost of ownership. Hosting on a cloud platform means practices always benefit from up-to-date technology, reduced downtime, and simplified expansion.
Fully Supported Transition and Integration
- Interfaces and Integrations:
- Standard HL7 and FHIR messaging supports local labs, hospital ADT feeds, and imaging facilities.
- eClinicalWorks and Aledade, Inc. announced a partnership to improve practice experience through enhanced EHR workflow and connectivity technology. Through this partnership, practices newly joining Aledade that use eClinicalWorks’ EHR will gain access to Sunoh.ai, an EHR-agnostic AI-powered scribe that enables physicians to capture and transcribe patient encounters in real-time. The new agreement builds on the in-depth partnership of data exchange and integration that already exists between Aledade and eClinicalWorks – a partnership that nationwide supports more than 400 practices that work with both companies. Aledade’s technology platform integrates with 100+ EHRs and practice management software (PMSs) – putting 300+ external data sources, such as hospital, lab, pharmacy, and claims data, all in one place, equipping you with knowledge to improve your patients’ health outcomes. Aledade also helps existing ACOs, IPAs, and networks optimize ACO performance while minimizing administrative inefficiencies.
- Custom Solutions:
- Organizations can connect custom or regional solutions, ensuring local workflows and preferences are supported alongside best-in-class national interoperability.
Conclusion
eClinicalWorks® empowers rural hospitals, critical access providers, and rural health centers to confidently transition to secure, interoperable, and user-friendly electronic health environments. With unparalleled national connectivity, industry-leading standards, patient-centered digital tools, and enterprise-grade security, eCW turns rural challenges into opportunities for innovation, collaboration, and better care.
Google Cloud
Contact: Melissa Hensley, HHS Lead, [email protected], 720-403-0549
Proposal 1: Cybersecurity
Google’s rural healthcare cybersecurity initiative
Cyberattacks on healthcare organizations disrupt their ability to operate and jeopardize patient care. Rural healthcare systems in the US serve 60 million people and are at the heart of countless communities. The safety of everybody in a community is threatened when critical healthcare information systems are unavailable due to cyber incidents.
Google is committed to helping vulnerable health systems strengthen their resilience to cyberattacks. We are partnering with government and industry to offer our services, support, and technologies, enabling systems to focus on patient care.
To prioritize data and technology to enhance cybersecurity
A tailored initiative to improve security, designed for rural hospitals
Rural health systems and hospitals reflect the uniqueness of the communities they serve, and so does our offer. It delivers a growing set of secure-by-design Google technology for access and collaboration, consulting, and support services, as well as security training resources at a discount or no cost. The solution is adapted to the needs of each rural health entity. The health facility should be located in a county or region designated as rural by the Health Resources and Services Administration (HRSA).
Leveraging the power of industry collaboration
Effective collaboration to defend against and respond to cyber attacks is vital to securing healthcare. Google is an ambassador partner to the Health Information Sharing and Analysis Center (Health-ISAC). Health-ISAC’s mission is to empower trusted relationships in the global healthcare industry to help prevent, detect, and respond to cybersecurity and physical security events so that members can focus on improving health and saving lives.
Program Offerings
Most of these will be offered at no cost or with significant discounts, acknowledging the financial constraints faced by many rural healthcare systems. Additionally, we will provide implementation services and support to eligible organizations.
Chrome Enterprise Browser and ChromeOS
To help health systems safely access and use internet-based and internal technology resources and deliver patient care, Chrome browser and ChromeOS offer a more secure alternative than other browser and operating system combinations.
Google Workspace
Google Workspace is a collaboration platform that pairs productivity applications (including Docs, Slides, Sheets, and Drive), messaging applications (such as Gmail and Chat), identity platforms (Cloud Identity Premium), and a suite of sophisticated security tools to help keep data safe. Workspace supports compliance with HIPAA and is used across hospitals and health systems globally.
Mandiant Education and Training Courses
To support education and training efforts, we’re making several on-demand and instructor-led cybersecurity courses available at no cost from our Mandiant Academy program.
Incident Response
Mandiant incident responders have been on the frontlines of the most complex breaches worldwide since 2004. Our incident response services are tailored to help clients understand the scope of, respond to, and recover from major incidents, while managing regulatory requirements and reputational damage. We’re making our incident response retainer service available to eligible rural healthcare entities at a reduced cost.
Proposal 2: Regional Collaborative Networks
Executive Summary
Regional “Collaborative” Networks: These networks focus on sharing resources and best practices among peer hospitals without a formal hub-and-spoke structure.
Case in Point: Wilderness Health (MN/WI) & Louisiana Independent Hospital Network Coalition: These coalitions of independent rural hospitals have successfully partnered to share staff, launch collective telehealth services (especially for mental health), and aggregate data for quality improvement initiatives.
Google Workspace: Serves as the communication and collaboration backbone for the entire coalition, allowing pharmacists, IT staff, and clinicians from different hospitals to work as a unified team.
Chronicle SecOps & Mandiant: A coalition could pool RHTP funds to purchase security services for the entire network, providing an enterprise-grade security posture that no single hospital could afford on its own.
Requirement: Recruit and Retain Clinicians
The rural healthcare workforce shortage is a full-blown crisis, undermining access to care in communities that need it most. This challenge is multifaceted, stemming from an aging clinical workforce, the immense difficulty of attracting new talent to remote areas, and high rates of burnout. Technology, when applied thoughtfully, can directly counteract these drivers of turnover. It can transform rural practice from an isolated, unsupported role into a connected, sustainable, and professionally rewarding career by reducing professional isolation, providing frictionless access to continuing education, and streamlining the administrative burdens that plague modern medicine.
Successful Models & Examples
Project ECHO (Extension for Community Healthcare Outcomes): A telementoring model that uses video conferencing to connect rural primary care providers with specialist teams from academic medical centers. They present de-identified cases and receive mentorship, effectively becoming local experts.
- Impact: Dramatically improves provider confidence and skills in managing complex conditions like Hepatitis C, chronic pain, and behavioral health. This reduces the feeling of isolation and burnout, which are key drivers of turnover.
Google Meet
The ideal platform for hosting ECHO clinics, with features like recording for asynchronous learning and breakout rooms for smaller group discussions.
Google Classroom/Sites: Can be used to create a resource portal for the ECHO participants, housing case presentation templates, clinical guidelines, and recorded sessions.
Virtual Scribes & AI-Powered Documentation:
A major source of physician burnout is administrative work and EHR documentation.
Impact: Offloading documentation to virtual scribes or using AI tools that listen to the patient encounter and auto-draft the clinical note can give providers back hours in their day, allowing them to see more patients or have a better work-life balance.
Technology Enablement: By leveraging Google Cloud’s foundational AI/ML APIs (e.g., Speech-to-Text, Natural Language API), the state can create a common technological backbone for ambient documentation. This allows the state to foster a competitive ecosystem of AI scribe vendors, avoiding lock-in to a single proprietary solution while ensuring all participating hospitals benefit from the same core, secure technology. RHTP funds can be used to procure both the platform and vendor services, delivering immediate relief from administrative burden across the state.
Requirement: Improve Health Outcomes & Promote Prevention/Chronic Disease Management
This requires shifting from reactive, in-person care to proactive, continuous engagement, particularly for patients with chronic conditions like diabetes, heart failure, and COPD.
Successful Models & Examples:
Remote Patient Monitoring (RPM) & Remote Therapeutic Monitoring (RTM): Using connected devices (blood pressure cuffs, glucometers, scales) to monitor patients at home and transmit data to care teams.
- Impact: This proactive model is the cornerstone of succeeding in value-based care arrangements. It allows for early intervention when a patient’s condition is worsening, preventing high-cost utilization (ER visits, readmissions) and improving quality metrics. It also empowers patients to become active participants in their own health, leading to better long-term outcomes and lower overall costs for the state.
Technology Enablement (Google’s Role):
- Google Cloud Platform (BigQuery, Looker): The ideal platform to ingest, store, and analyze the massive amounts of data generated by RPM devices. A state could build a centralized monitoring dashboard for a regional network of care managers.
- Google Workspace (Chat, Meet): These are the tools used by care managers to communicate securely with patients when their data indicates a potential issue.
- Community-Based Wellness Programs with Digital Support: Leveraging community health workers (CHWs) and local organizations (schools, churches) to promote healthy behaviors, supported by digital tools.
- Case in Point: The Chronic Disease Self-Management Program (CDSMP): An evidence-based program that uses workshops (which can be delivered virtually) to teach patients skills for managing their chronic conditions.
- Technology Enablement (Google’s Role):
- Google Forms & Sheets: To manage program registration, track attendance, and collect outcomes data.
- YouTube: To host a library of on-demand health education videos for program participants.
- Google Maps Platform: To help CHWs plan their routes and identify community resources (e.g., food banks, safe walking trails).
By incorporating these proven, technology-centric models into a state’s RHTP application, you can provide a compelling, evidence-based plan that is highly likely to be funded by CMS.
Proposal 3: Data solutions
Executive Summary
- Addressing RHTP Requirement: Prioritize data and technology-driven solutions that help rural providers furnish health care services as close to the patient’s home as possible, including by improving cybersecurity.
- Google recognizes that cybersecurity is no longer an IT issue; it is a patient safety and financial stability issue. Recent cyberattacks have crippled hospitals nationwide, and our rural facilities are particularly vulnerable due to limited resources and staffing. To address this, our plan dedicates a significant portion of RHTP funding to establish a statewide Rural Hospital Security Fabric, powered by Google Cloud.
This program will provide every eligible rural facility in states with:
- Google Workspace Enterprise: To protect our primary communication channel—email—from phishing and malware, while enabling secure collaboration (telehealth, remote work) for clinical staff.
- Chrome Enterprise Premium: To ensure that every device (hospital-owned or personal) used to access patient information is protected with advanced threat and data loss prevention.
- Mandiant Incident Response & Training: To provide our hospitals with on-demand access to elite cybersecurity experts in the event of an attack, and to upskill local IT staff, addressing the critical workforce gap.
- Managed Security Services: Through our partners [CloudWave/Netenrich], we will provide 24/7 security monitoring and management, relieving the burden on local hospital staff. This comprehensive security investment will immediately reduce the risk profile of our entire rural health network, protecting patient data and ensuring the continuity of care.
- Addressing RHTP Requirement: Initiate, foster, and strengthen local and regional strategic partnerships…to promote quality improvement, increase financial stability, [and] maximize economies of scale.
Our plan leverages a statewide technology platform to create unprecedented economies of scale. By centrally procuring this foundational technology from Google Cloud for all eligible rural facilities, [State Name] can provide enterprise-grade tools at a fraction of the cost.
This statewide approach will foster collaboration by:
- Creating a Common Platform: All rural providers will use the same secure collaboration tools (Google Workspace), making it easier to share best practices, coordinate patient transfers, and manage regional population health initiatives.
- Enabling Regional Data Sharing: Using Google Cloud Platform’s secure and interoperable data solutions, we will create a framework for regional health information exchange, allowing providers to have a more complete view of their patients’ health, reducing duplicative tests and improving care coordination.
Section 3: Budget and Solution Packaging
- The following represents a sample budget allocation for the technology component of your RHTP application.
- This is based on a per-hospital model and can be scaled to cover all eligible facilities in [State Name].
- Per-Hospital Annual Cost Estimate (Based on 250 users):
Estimated Annual Cost
- Google Workspace & Chrome
- Secure productivity and endpoint security for 250 users.
- $30,000
- Mandiant & Security Platform
- IR Retainer, Training, SecOps Platform Access
- $50,000
- Partner Services
- Deployment, Migration, and Managed Security Services.
- [To be quoted by partner]
- Total Per-Facility Cost ~$80,000 + Partner Fees
Harbor
Kevin Lavelle, CEO and Cofounder, [email protected]
Executive Summary
Harbor is a next-generation monitoring and remote patient care company that began as a family-focused monitoring platform and quickly expanded into Medicaid and rural health contexts. We have developed patent-pending hardware supported by real-world remote patient monitoring (RPM) services.
Harbor has shipped more than 10,000 devices nationwide and deployed RPM services to over 100 families, including medically complex rural households. Our solution combines a dedicated 10-inch display with edge-based AI monitoring and a Remote Patient Monitoring program, where trained staff provide overnight monitoring and escalate to caregivers or clinicians only when needed.
Harbor delivers high-impact support to families and providers while solving systemic challenges:
- $40-50 per night vs. $200–$300 per night for in-home staff — a 4–7.5x cost advantage
- Average hospital readmission costs range from $10,000 to $100,000+ per event — preventable with proactive monitoring
- Caregiver burnout reduction, allowing families to sustain care at home instead of institutionalizing loved ones
- Hospital-to-home integration, reducing readmissions that jeopardize rural hospital solvency
Harbor is shovel-ready for inclusion in state Rural Health Transformation Plans and aligns with CMS scoring criteria: it addresses statutory buckets, has measurable outcomes, and is sustainable beyond the RHTF through Medicaid RPM reimbursement and MCO partnerships.
The Rural Challenge
- Staffing crisis: In rural areas, overnight or respite staff are scarce and prohibitively expensive. Families often face months-long gaps in coverage.
- Financial strain on hospitals: Preventable readmissions or ER visits average $10k–$100k+ each. Rural hospitals cannot sustain these losses.
- Caregiver burnout: Families without respite support are forced into crisis, often institutionalizing patients earlier than necessary.
The Harbor Solution
Harbor provides a privacy-first, patent-pending monitoring system paired with human-powered remote services. Our system addresses multiple statutory goals:
- Improve access: Families in rural counties gain access to overnight support without needing scarce in-home staff.
- Improve outcomes: Patients remain safe at home, avoiding preventable hospitalizations.
- Chronic disease prevention/management: Continuous monitoring identifies issues early and escalates only when necessary.
- Partnerships: Rural hospitals and MCOs can extend reach into homes through Harbor, creating regional hub-and-spoke coverage.
- Financial stability: By reducing readmissions, Harbor strengthens rural hospital margins.
- Data-driven care: Harbor provides measurable metrics at the county level, allowing states to track impact.
Proposed Initiatives for State Plans
Harbor proposes three shovel-ready modules that states can include in their RHTF applications:
1. Rural RPM & Respite Network
- Deploy Harbor devices to medically complex children, adults with disabilities, and post-acute patients.
- Overnight coverage at $40-50/night provides families rest and reduces hospital utilization.
2. Hospital-to-Home Readmission Reduction
- Rural hospitals deploy Harbor for high-risk discharges (30–90 days).
- Expected outcome: 20–30% reduction in readmissions, saving $10k–$100k+ per avoided hospitalization.
3. Caregiver Sustainability Program
- RHTF-funded respite monitoring to prevent caregiver burnout.
- Expected outcome: Increased caregiver retention, lower rates of institutionalization, and improved quality of life.
Measurable Outcomes
Harbor’s model allows states to track impact at the county level:
- Readmission rates (baseline vs. intervention)
- ED visit frequency per 100 patient-months
- Caregiver burden surveys before and after intervention
- Number of respite nights delivered at $50 vs. $250 baseline
- Total avoided hospitalization costs ($10k–$100k+ per prevented event)
Sustainability Beyond RHTF
Harbor is designed to persist past the 5-year fund:
- Medicaid reimbursement: States can align Harbor with RPM and respite care codes, locking in substantial ongoing savings vs. alternative methods of care.
- MCO integration: Harbor reduces per-member-per-month costs and aligns with value-based care contracts.
- Hospital partnerships: Rural hospitals can use Harbor to stabilize margins by reducing readmissions.
Policy Levers for States
To maximize CMS scoring, states can pair Harbor with policy changes such as:
- Expanding RPM coverage for special needs and respite use cases
- Ensuring telehealth parity for remote monitoring escalation
- Allowing directed payments to FQHCs/CAHs deploying RPM technology
Conclusion
Harbor provides a proven, scalable, and cost-effective model that addresses rural access, outcomes, hospital solvency, and caregiver sustainability. With over 10,000 devices shipped, 100+ families served in RPM contexts, and demonstrated cost advantages, Harbor is ready to help states deliver measurable, sustainable rural health transformation under the RHTF.
Health Recovery Solutions (HRS)
Contact: Sudeep Pisipaty, Chief Commercial Officer, [email protected], 732-763-6188 (cell) 347-699-6477 (office)
Executive Summary
HRS brings extensive experience supporting rural hospitals and health systems through Remote Patient Monitoring (RPM), Chronic Care Management (CCM), Hospital at Home, and virtual care programs – having served over 1M patients. These solutions are designed to improve hospital throughput, optimize patient flow, enhance staffing efficiency, bridge access gaps, and create sustainable models of longitudinal care.
Problem
Rural health care delivery faces persistent challenges related to access, capacity, and staffing. Geographic isolation, limited specialty services, and broadband barriers leave many rural residents unable to receive timely care. Hospitals experience high rates of preventable readmissions and emergency utilization, straining limited inpatient capacity. Workforce shortages exacerbate these pressures, forcing clinicians to manage too many patients with too few resources. Without intervention, these challenges perpetuate inefficiency, poor outcomes, and financial strain.
Solution
HRS’s model is built to address these challenges directly. Our PatientConnect® RPM platform enables providers to monitor patients after discharge, detect early warning signs, and intervene before hospital-level care is required. In one major health system, implementation of HRS technology achieved a 71 percent reduction in CHF readmissions. Another health system demonstrated a 73 percent relative reduction in 30-day all-cause readmissions for CHF patients, decreasing rates from 19.3 percent to 5.2 percent over three years. These measurable outcomes show how RPM prevents unnecessary hospitalizations, improves patient flow, and allows rural hospitals to serve more patients with existing resources.
Hospital at Home is a core capability within the HRS portfolio. For appropriate patients, Hospital at Home enables earlier discharge and the delivery of hospital-level care in the home, supported by continuous monitoring, daily telehealth visits, and coordinated logistics for labs and medications. One health system transitioned more than 2,500 patients and freed over 13,000 inpatient bed days through Hospital at Home. In rural hospitals, where bed capacity is extremely limited, this level of relief significantly enhances throughput and ensures timely access for other patients in need.
Avera Health provides further evidence of the impact on throughput and access. Serving rural communities across five states, Avera leveraged HRS telehealth and RPM to manage patients safely at home. Over the course of seven months, nearly 3,500 patients were monitored with a hospitalization rate of only 6.1 percent and an emergency visit rate of 7.9 percent. Patient satisfaction exceeded 95 percent. By reducing acute utilization, conserving hospital resources, and maintaining high satisfaction, this program demonstrates how HRS can support rural systems under strain while bridging significant gaps in access.
Workforce efficiency is also central to the HRS approach. Rural hospitals often face severe staffing shortages, and burnout contributes to further attrition. HRS alleviates these pressures by shifting routine surveillance and engagement to virtual platforms. Automated surveys, biometric alerts, and condition-specific education allow clinicians to focus on patients who need escalation. Our CareConnect service supplements local capacity with centralized, 24/7 monitoring support, ensuring continuity of care during workforce shortages or demand surges. These measures extend the reach of rural clinicians, stabilize retention, and create more sustainable staffing models.
Beyond immediate operational improvements, HRS supports the transition to longitudinal care. RPM provides continuous biometric data over months, while CCM offers structured outreach, medication management, and care coordination for patients with multiple chronic conditions. This combination closes gaps that often lead to cycles of hospitalization and relapse. One health system achieved over $5 million in cost savings within six months while sustaining an 83 percent reduction in readmissions through combined RPM and CCM. For rural communities, this model ensures that patients remain supported long after discharge, reducing the burden on hospitals while improving quality of life.
Regulatory alignment is a critical element of successful program implementation. National experts have emphasized the importance of selecting remote monitoring vendors that meet strict standards for HIPAA compliance, FDA-cleared devices, transparent patient consent, and secure data management. HRS adheres fully to these standards, providing encrypted data transmission, secure storage, and documented consent workflows. Our compliance framework enables hospitals to implement RPM with confidence, minimizing legal and operational risk.
Financial sustainability is another priority for rural systems. Recent CMS policy changes allow Rural Health Clinics and Federally Qualified Health Centers to bill for individual RPM and CCM codes, replacing the previous bundled approach. This change improves reimbursement accuracy and creates a predictable revenue stream to support long-term program operations. For rural hospitals with limited margins, this alignment of clinical transformation and reimbursement is a core value proposition. HRS works closely with partners to operationalize billing pathways and ensure that programs are both clinically effective and financially viable.
Interoperability further strengthens outcomes. HRS integrates with leading EMR systems, including Epic and Cerner, ensuring that patient vitals, alerts, and notes flow directly into provider workflows. This eliminates duplicative data entry, enhances communication across care settings, and provides real-time population-level dashboards. These dashboards enable hospital leaders and state agencies to monitor engagement, readmission rates, and utilization patterns, ensuring accountability and informing evidence-based decision-making.
Equity is embedded in the design of HRS programs. Cellular-enabled devices extend access to patients in areas without broadband, while multilingual educational content and culturally tailored care pathways improve engagement in diverse populations. For example, Spanish-language diabetes pathways have demonstrated measurable improvements in A1C and blood pressure among underserved patients. Caregiver integration ensures that families remain engaged in supporting patients, further closing gaps in access.
The combined impact of this comprehensive model is significant. Hospitals reduce readmissions, shorten lengths of stay, and free bed capacity. Patients gain continuous access to care despite geographic, financial, or technological barriers. Clinicians operate more efficiently, supported by streamlined workflows and centralized monitoring. State agencies gain transparent reporting on utilization and outcomes. Most importantly, rural communities achieve greater health equity and sustainability.
Over a three-year period, HRS anticipates that hospitals using these models will achieve 30 to 50 percent reductions in readmissions and emergency visits, significant improvements in chronic disease outcomes, and six-figure annual savings per participating hospital. These outcomes are achievable because they have already been demonstrated across large integrated systems, academic centers, and rural multi-state networks.
Conclusion
In conclusion, HRS offers a proven framework aligned with the Rural Health Transformation Program’s goals. Our programs improve throughput, optimize staffing, and expand access while enabling longitudinal care and ensuring financial sustainability. By combining RPM, CCM, Hospital at Home, and regulatory compliance into an integrated model, HRS equips rural hospitals to overcome current challenges and build a stronger, more equitable health system for the future.
Hopscotch Primary Care
Contact: Finn Kennedy, 8VC, [email protected], 917-751-0264
Transforming Rural Health Through Technology-Enabled Primary Care
Submitted by: Hopscotch Primary Care (Tim Gronniger, CEO)
Executive Summary
- A rural clinic may need 25 visits a day to break even. In many towns, it sees fewer than 15. The gap pushes providers out and leaves patients with no option but to travel long distances or wait until conditions spiral into ER visits. Hopscotch is the only scaled, technology-enabled primary care model built specifically for rural America.
- We operate 11 clinics across western North Carolina that care for more than 15,000 patients (predominantly Medicare) in communities as small as 1,500. Our model delivers measurable results: 4.3-STAR quality, 90+ NPS, and a ~30% reduction in medical loss ratio for patients two years into care.
- With support from the Rural Health Transformation Fund, we can expand to 16+ clinics serving >20,000 residents on a shared data platform and outcomes-based contracts. We request $15M over five years (breakdown below) to replace episodic, facility-centric spending with durable, local, primary care capacity.
Problem
- Rural residents are far more likely to end up in the hospital for conditions that should have been managed in primary care. Preventable admissions are 40% higher than in cities, and nearly one in three rural residents lives with multiple chronic conditions.
- At root, the problem is access. Rural communities have fewer doctors, fewer clinics, and fewer options close to home. Primary care supply averages 46 physicians per 100K people in rural areas versus 61 in urban markets. Specialist supply is even more scarce, with 30 per 100K in rural America compared to 263 in cities. When local care isn’t available, problems that should be caught early are left to worsen until an ER visit is the only option.
- Hospitals, often the only remaining access point, are themselves fragile. Nearly 200 rural hospitals have closed in the past two decades, and more than 700 are at risk. Many run below capacity, depend heavily on subsidies, and focus on acute care rather than prevention. As they cut services or shut down entirely, communities lose not just hospital beds but imaging, diagnostics, and routine follow-up.
- Older and poorer populations feel the effects most. 18% of rural residents are over 65, compared to 14% in cities, and 15% live below the poverty line. Medicaid covers nearly a quarter of rural residents, yet local clinics rarely have the resources to help patients stay enrolled and connected to care. The result is a cycle of missed prevention, worsening chronic disease, and costly hospitalizations could have been avoided.
- Without a new operating model that can sustain clinics in small towns and pay for outcomes rather than volume, this cycle will only accelerate.
Our Model
- Hopscotch replaces fee-for-service with risk-bearing primary care designed for small towns. Clinics are staffed by integrated teams (a physician, an advanced practitioner, a nurse, a care manager, and a community health worker) who manage a panel of roughly 1,200 – 1,500 patients. This structure keeps care local while giving each patient more touchpoints than a single clinician could provide.
- Each clinic runs on a single software system that pulls records from hospitals and payers, highlights missed cancer screenings or blood pressure checks, and prepares notes before each visit. That cuts down paperwork and allows clinicians to spend more time with patients.
- When patients need a specialist, they don’t have to drive two hours to the nearest city. Each Hopscotch clinic has a dedicated room with high-speed Starlink connectivity, where patients can see a cardiologist, psychiatrist, or other specialist virtually. Appointments that used to take months and long travel can now happen the same week, in the same building where they see their primary care doctor.
- For high-risk patients, remote monitors track weight, blood pressure, or glucose at home. Sudden changes trigger an alert, and the care team steps in before it becomes an ER trip.
- Hopscotch doesn’t bill by the visit. We contract with Medicare Advantage plans and ACOs under risk-based agreements that pay for outcomes. That means we can call patients after a hospital stay, schedule same-week follow-ups, or add a behavioural health consult without worrying whether it generates a billable code.
- For patients, this means timely access, fewer long drives, and problems caught before they escalate. For clinicians, it means working in teams that let them practice at the top of their license. For taxpayers and payers, it means fewer preventable admissions and a sustainable way to keep care local in rural communities.
Evidence to Date
The model is already working in western North Carolina. Across 11 clinics serving more than 15,000 patients, mostly Medicare, results are consistent:
- Quality: 4.3 STAR composite ratings with strong performance on prevention and screening measures
- Patient experience: Net promoter score above 90, with more than 90% of patients staying in the model year to year.
- Utilization and cost: Patients who have been with Hopscotch for two years show about a 30% reduction in medical loss ratio, driven by fewer avoidable admissions.
- Workforce: More than 50 clinicians recruited to rural town in 24 months.
- Economics: Contribution margins improve by roughly $200 PMPM over three years, and clinics breakeven in about four years.
These outcomes show that high-quality, financially sustainable primary care is achievable in rural markets and is ready to scale.
Implementation Plan
- Year 1-2:
- Open new clinics in the highest-need rural counties. (Category 1: Access)
- Partner with existing PCPs and hire additional PCPs to staff clinics, supporting them with a localized and distributed workforce (e.g., Community Health Workers, CMRNs, Insurance Navigators) with access to virtual specialists (Cat 2: Outcomes, Cat 3: Prevention)
- Deploy advanced AI analytics to care teams, allowing them to focus on the sickest patients, and supplement clinic infrastructure with Starlink to provide our rural patients access to reliable broadband (Cat 6: Data/Tech)
- Year 3-5:
- 5+ total clinics, 20k+ total residents served. (Category 1: Access)
- Recruit 30+ PCPs to practices with 4+ year commitments. (Cat 5: Workforce)
- Market is cash flow breakeven and able to sustain new clinic growth without incremental outside investment. (Category 7: Solvency)
- Mutually beneficial partnerships with local rural hospitals and with local community organizations [Cat 4: Partnerships and Cat: 8 closure risk]
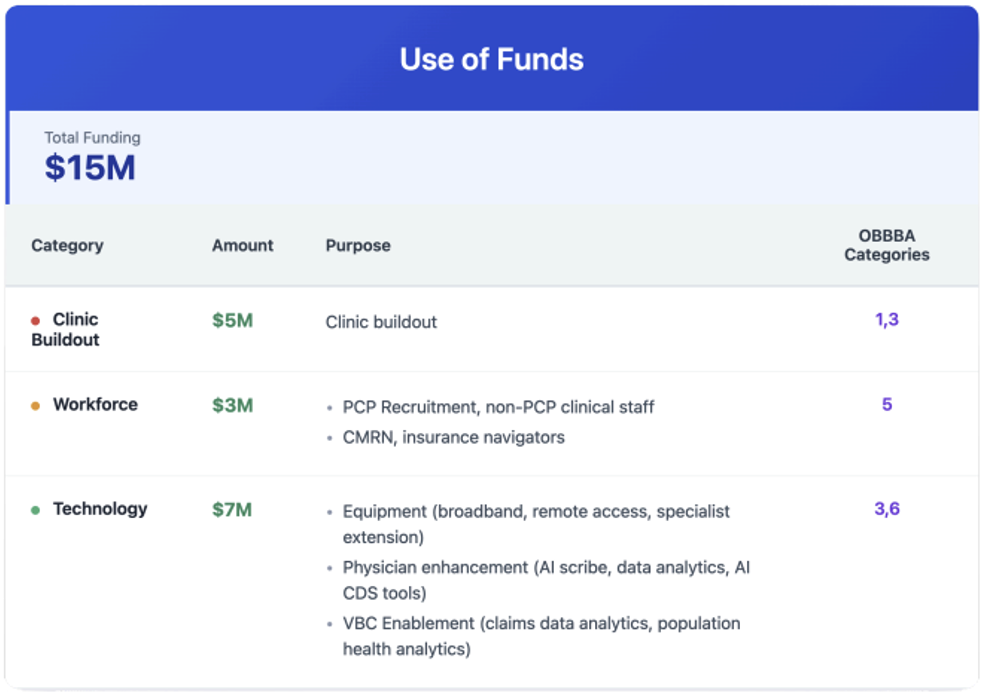
Measurement and Guardrails
- Patient access:
- Patient encounters reporting – number of patients impacted. Validated through EMR data.
- Outcomes
- STARS reporting
- Patient Net Promoter score – to show quality of service and patient feedback. Internally captured, but queried through all
- Medical Loss Ratio reporting – validated through third-party payer reports
- Workforce metrics
- PCPs are hired in community; able to validate through payroll records
- Jobs are created and filled; able to validate through payroll and state tax records
Conclusion
- Rural communities can’t sustain care on visit-based economics. The result is clinic closures, fragile hospitals, and patients turning to the ER for problems that should have been caught upstream.
- Hopscotch proves rural care can be sustained when clinics are local, teams are integrated, technology supports prevention, and payment rewards outcomes.
- With the Rural Health Transformation Fund, states can extend a proven model that keeps care close to home, improves health outcomes, and lowers costs across rural America.
Categories Addressed
- Access: New rural clinics, same/next-day appointments, virtual specialty care.
- Outcomes: High-risk programs, fewer preventable admissions, improved STARs.
- Technology & Prevention: Unified software, Starlink, remote monitoring
- Partnerships: Hospital and provider agreements for ER diversion
- Workforce: Recruitment, retention, and team-based care.
- Data: Interoperable records and payer data feeds.
- Solvency: Risk-based contracts, glidepath funding, sustainable economics.
- Closure Risk: Support for fragile hospitals, shift avoidable volume to primary care.
Nest Health
Home-Based Family Primary Care for Rural Communities
Contact: Paige Franklin, VP Growth, 270-871-3928, [email protected]
Executive Summary
Nest Health proposes implementing our proven home-based, family-centered primary care model to transform health outcomes in rural communities. Our approach delivers comprehensive primary care directly to households, eliminating transportation and scheduling barriers that disproportionately affect rural families. With demonstrated results including significant reduction in emergency department visits and per member per month savings across managed Medicaid members, this model directly addresses rural health disparities while generating sustainable cost savings.
The Rural Health Challenge
Rural communities face unique barriers to accessing quality primary care: limited provider availability, long travel distances, transportation challenges, and fragmented care delivery. These obstacles lead to delayed preventive care, unmanaged chronic conditions, and avoidable emergency department utilization. Rural families, particularly those with multiple children, struggle to coordinate care across different providers and locations, resulting in gaps in essential services like well-child visits and maternal health screening.
Nest Health’s model eliminates structural barriers by bringing multidisciplinary care teams directly to rural households. Our comprehensive approach includes in-home visits by advanced practice clinicians, nurses, behavioral health specialists, and community health workers who deliver family-centered care serving multiple household members in single visits. This model provides 24/7 clinical access, including triage lines and same-day urgent care, ensuring rural families have immediate support when needed.
The care delivery framework integrates behavioral health screening and referral, including maternal depression screening, with standardized social needs screening that includes referrals to services such as WIC, housing support, and food assistance. Longitudinal care coordination spans child and adult care, behavioral health, and social supports, creating a seamless healthcare experience for rural families.
Our target population includes rural households with at least two members, with one having no primary care visit in 6-12 months, as well as evidence of high preventable spending, such as chronic conditions or multiple emergency department visits. These households face significant geographic barriers to traditional clinic-based care, making them ideal candidates for home-based intervention.
Partnership development forms the foundation of our implementation approach. We collaborate with state Medicaid agencies and managed care organizations to identify counties with the highest need and readiness for implementation. This phase includes establishing data sharing agreements and completing provider credentialing processes necessary for program launch. Infrastructure development follows partnership establishment, where we deploy multidisciplinary care teams with designated rural coverage areas and implement electronic health record systems with real-time care coordination capabilities. This phase also includes establishing 24/7 clinical support infrastructure to ensure continuous access for rural families. Currently, we operate under active contracts with three Medicaid managed care plans in two states, providing a proven foundation for expansion.
Our value-based payment model combines monthly primary care payments based on preliminarily assigned households with fee-for-service payments for delivered services. Two-sided risk arrangements tie shared savings to cost reduction and quality improvements, ensuring alignment between provider incentives and program goals. Performance will be measured across core indicators that demonstrate meaningful health improvements, including well-child visit completion rates (W30, WCV), prenatal and postpartum depression screening (PND-E, PDS-E), and follow-up after hospitalization (FUH). Additionally, we track emergency department utilization reduction, as well as both patient and caregiver experience scores, to ensure comprehensive quality assessment.
The model’s financial sustainability stems from demonstrated cost savings that exceed program investment. Our value-based payment structure aligns incentives for quality and efficiency, while enhanced federal matching through innovative Medicaid authorities provides additional financial support. The program also creates workforce development opportunities, generating rural employment for healthcare professionals and strengthening local economic development. This approach uniquely addresses rural challenges by eliminating travel barriers through home-based delivery and maximizing provider efficiency through household-level care. The model strengthens community ties via local workforce development while improving care coordination for geographically dispersed services. Rural working families particularly benefit from reduced time away from employment, as care comes to them rather than requiring travel to distant facilities.
Conclusion
Nest Health seeks partnership with states developing Rural Health Transformation Plans to implement this evidence-based, family care model. We offer proven care delivery infrastructure and protocols, experienced multidisciplinary care teams, and comprehensive data systems for outcome measurement and reporting. Our technical assistance for Medicaid integration includes ongoing quality improvement and provider training to ensure successful program implementation. Home-based family care represents a transformative approach to rural health challenges, directly addressing access barriers while improving outcomes and reducing costs. With established evidence of success and scalable infrastructure, Nest Health is positioned to be a key partner in rural health transformation efforts nationwide.
OnMed
Contact: Carrie O’Rourke, General Manager, [email protected]
Executive Summary
OnMed proposes a practical, market-based way for states to meet the Rural Health Transformation (RHT) objectives under the One Big Beautiful Bill Act by building a rural access network anchored in clinic-grade telehealth care stations. These private, life-sized rooms deliver live clinician visits with integrated diagnostics—such as stethoscope, otoscope, blood pressure, and dermatologic/ENT imaging—alongside e-prescribing, lab and imaging orders, referrals, and full EHR/FHIR interoperability. Placed in trusted community settings—FQHC satellites, critical access hospitals, community colleges, libraries, EMS/fire stations, and behavioral health clinics—the stations bring comprehensive care as close to home as possible, without requiring on-site clinical staff.
The experience is ADA-compliant, multilingual, and connectivity-resilient, with primary broadband and satellite failover. In a single design, the model directly addresses OBBA’s priorities: it expands access, improves outcomes, prioritizes new technology for prevention and chronic disease management, strengthens local partnerships, grows the workforce through new roles and training pathways, advances data-driven care near the patient, and supports long-term hospital solvency by preserving appropriate referrals and lowering avoidable high-cost utilization.
Syntasa
Contact: Mo Arora, VP Sales, [email protected], 1-647-284-3521
Proposal 1
Executive Summary
Commitment to Rural Health Transformation
The One Big Beautiful Bill Act (OBBA) established the Rural Health Transformation Fund (RHTF) to empower states to create sustainable, technology-driven improvements to rural care. Google Public Sector and Syntasa are deeply aligned with this mission and propose IMPACT (Intelligent Management, Prevention, and Analytics for Chronic Transformation) as a targeted program addressing OBBA Category #3: Prioritizing new and emerging technologies that emphasize prevention and chronic disease management.
Chronic diseases such as diabetes, hypertension, COPD, and CHF disproportionately burden rural communities. Current models often rely on reactive treatment instead of prevention. IMPACT will change this trajectory by deploying advanced Data + AI solutions that make prevention actionable, measurable, and sustainable at scale.
Google Public Sector Strengths
Founded in June 2022, Google Public Sector delivers cloud technologies to public sector institutions across the U.S. With expertise in secure data integration, analytics, and modern cloud adoption, Google Public Sector has supported agencies nationwide in building actionable, scalable health and social-service insights.
Representative work includes:
- CHNA 2.0 (Wayne State University and City of Dearborn): Real-time chronic disease analytics.
- AI-first Provider Locator (AHCCCS): Matching residents with care quickly through AI-powered tools.
- Provider Analytics (AHCCCS): Benchmarking provider performance for quality improvement.
- Substance Use Analytics (Oklahoma ODMHSAS): Forecasting opioid surges with predictive analytics.
- These cases demonstrate Google’s ability to rapidly scale secure, AI-driven tools that strengthen outcomes and community engagement.
Syntasa
Since 2014, Syntasa has specialized in health transformation analytics for the U.S. public sector. As a Google Premier Partner, Syntasa brings specific expertise in rural and public health transformation, including:
- Chronic disease insights and provider performance benchmarking
- Substance use and opioid analytics across multiple states
- Behavioral health dashboards integrated with demographic and community-level data
- The Syntasa Data + AI Platform is pre-configured for common public health data formats, accelerating the timeline from concept to measurable results. By integrating clinical data with community and digital behavior signals – search patterns, social media, surveys – Syntasa provides forward-looking prevention insights to anticipate rural health challenges before they escalate.
Proposed Program – IMPACT
IMPACT is a Rural Chronic Disease Analytics Platform that applies emerging technologies to proactively prevent and manage chronic illness in rural settings.
Core Capabilities:
- Predictive Hotspot Maps: Detect geographic and community-level risks for chronic disease escalation.
- AI-driven Trend Forecasting: Monitor lab metrics (e.g., A1C, blood pressure) alongside social and behavioral data to predict future care needs.
- Consumer-Facing Integration: Deliver tailored insights for rural patients and caregivers, supporting telehealth adoption and chronic care self-management.
- Equity-by-Design Analytics: Incorporate rural-specific social determinants, helping states target interventions for high–Social Vulnerability Index (SVI) communities.
This program directly responds to OBBA’s intent by using new and emerging technology not just to monitor health, but to shape healthier futures through proactive engagement.
What Sets Us Apart
- Pre-Built Accelerators for Chronic Disease: Configured to ingest state-level data quickly and turn it into prevention dashboards in weeks, not years.
- Predictive Modeling and Anomaly Detection: Delivers early-warning systems for states to prevent crises and reduce costs.
- Behavior-to-Outcome Linkage: Unique methodology integrating digital behavior data (search/social) with health outcomes to uncover unmet prevention needs.
- Proven Scalability: Deployments across multiple states demonstrate rapid results, replicable and extensible nationwide.
Expected Outcomes and Success Measures
Short-Term (0–12 months):
- Achieve 90% ingestion of chronic disease data into a unified model.
- Launch prevention dashboards, reducing time-to-insight from months to days.
- Demonstrate 100% utilization across pilot districts, measured by dashboard queries and provider engagement.
Mid-Term (12–36 months):
- Improve chronic care control by 8–12% (e.g., A1C, blood pressure).
- Cut avoidable ED visits/readmissions for chronic conditions by 10%.
- Increase preventative screenings and care uptake in rural high-SVI ZIP codes.
Long-Term (36–60 months):
- Sustain reduced chronic disease burden and narrow rural-urban disparities.
- Scale IMPACT into future OBBA-aligned domains (e.g., maternal care, behavioral health).
- Establish IMPACT as the state’s long-term, reusable platform for data-driven chronic disease prevention.
Draft Implementation Plan
Phase 1 – Launch (0–12 months): Deploy IMPACT within the state’s Google Cloud tenancy, integrate datasets, and create initial disease surveillance dashboards.
Phase 2 – Enhance (12–36 months): Add predictive modeling, anomaly detection, and consumer-facing engagement tools. Train providers in applying insights.
Phase 3 – Scale (36–60 months): Expand platform statewide; add new chronic disease categories and additional CMS activity areas. Transfer analytic capacity to state staff.
Sustainability Plan
Governance: Hosted within state-controlled GCP tenancy for compliance, with features like Assured Workloads, CMEK, and PHI/PII masking to ensure HIPAA and CMS alignment.
Capacity-Building: Documentation, knowledge transfer, and analyst onboarding ensure state teams can independently manage and extend dashboards.
Financial Model: Designed for reuse across multiple CMS-approved activities, maximizing OBBA and federal funding impact.
Scalability: Flexible framework allows rapid addition of maternal health, cancer prevention, oral health, or behavioral conditions.
Success Stories from Past Programs
- Dearborn, MI (CHNA 2.0): Integrated Census, social media, and city data for real-time chronic disease monitoring; Generative AI on Google Vertex reduced analysis time from months to days.
- Oklahoma (Substance Analytics): Predicted trends in opioid use by integrating community-level datasets.
- Arizona (Provider Dashboards): Delivered ongoing performance metrics that improved clinician quality of care statewide.
These examples prove the Google + Syntasa team’s ability to deliver scalable prevention-focused programs aligned to OBBA’s Category #3 priority.
Organization Descriptions
Google Public Sector: Subsidiary of Google LLC, launched 2022, delivering secure Google Cloud technologies to the U.S. public sector. Supports data-driven transformation for federal, state, and local governments.
Syntasa: Google Premier Partner founded in 2014 and is headquartered in Washington, D.C. It specializes in substance abuse analytics, chronic disease dashboards, behavioral health, and provider performance. Its Data + AI platform uniquely integrates outcome, community, and digital behavior data for predictive prevention.
Closing Path Forward
The OBBA represents a historic opportunity to shape rural health for the next generation. With IMPACT, states gain a proven, scalable, and evidence-based solution to leverage OBBA funding for durable transformation in chronic disease prevention. Google Public Sector and Syntasa stand ready to support policymakers, Medicaid directors, and rural stakeholders in designing, implementing, and sustaining this vision.
Proposal 2
Executive Summary
Google Public Sector and Syntasa propose a consumer-facing, AI-enabled healthcare navigation and analytics solution that places high-quality care within reach of rural residents.
This initiative is designed to ensure rural hospitals and local providers can leverage modern data and technology to extend services closer to home, while also providing real-time insights to state leaders for smarter, data-driven decisions.
Our approach unites secure data integration, AI-powered care navigation, and predictive analytics to make rural healthcare more accessible, efficient, and sustainable. It directly meets the intent of OBBA category six: prioritizing technology-driven transformation that helps rural providers deliver better care without requiring patients to travel long distances.
Proposed Initiative: AI-Enabled Rural Health Resource Platform
We propose launching a scalable, cloud-based platform that provides two interconnected capabilities:
Consumer Navigation Tool: An intuitive virtual assistant, available on web and mobile, that helps rural patients locate nearby providers, including primary care, mental health, substance use treatment, and chronic disease management. It offers conversational, multilingual guidance and real-time availability so residents can quickly connect with local services.
Provider Analytics Backbone: A suite of dashboards for rural hospitals, providers, and administrators that highlights treatment deserts, benchmarks provider effectiveness, and identifies gaps in coverage. These insights allow leaders to strategically adjust care delivery and ensure resources reach underserved communities.
Potential Impact on Rural Health
For Patients:
- Simplifies the process of locating healthcare providers in their own community.
- Cuts search and referral times dramatically, shifting from weeks of uncertainty to minutes.
- Provides accessible explanations of treatment options, particularly for chronic disease, behavioral health, and substance use.
For Rural Hospitals and Providers:
- Equips local systems with near real-time analytics on patient demand, provider performance, and unmet needs.
- Improves operational efficiency by reducing unnecessary ER visits and guiding patients toward preventive or primary care.
- Strengthens financial sustainability through better resource alignment and data-informed planning.
For State Leadership:
- Establishes a durable, reusable data backbone that supports CMS rural health transformation plans.
- Supplies predictive analytics that forecast emerging rural health needs.
- Ensures long-term sustainability with infrastructure that can be adapted for additional initiatives, such as maternal health or cancer screening.
Success Stories and Prior Experiences
Google Public Sector and Syntasa have partnered with state health systems to modernize access and analytics using similar technology:
- Arizona: Built an AI-powered treatment locator to address the opioid epidemic, transforming a static provider list into a dynamic, real-time portal that connected citizens to addiction treatment and Naloxone resources.
- Georgia: Unified statewide opioid and behavioral health data into dashboards and consumer resource maps, enabling both residents and agencies to track and improve treatment.
- Oklahoma: Delivered real-time integration of demographic, dispatch, and overdose data, empowering state leaders to launch microtargeted interventions and reshape their behavioral health response.
Each of these examples demonstrates our ability to implement scalable, technology-driven solutions that empower both patients and local healthcare providers.
Implementation Plan
Short-Term (0–12 months):
- Gather and normalize existing state health and provider data.
- Launch pilot AI-enabled navigation tool in targeted rural communities.
- Success measure: reduced time for patients to find appropriate services; early adoption confirmed by usage metrics.
Mid-Term (12–36 months):
- Expand platform statewide, incorporating patient feedback and additional data streams such as provider capacity and patient outcomes.
- Deploy data dashboards to rural hospitals and administrators for real-time gap analysis.
- Success measure: measurable increases in care connections and reductions in preventable ER admissions.
Long-Term (36–60 months):
- Integrate predictive analytics to forecast rural health demand at the community and county levels.
- Scale for future health priorities (maternal health, cancer screening, preventive outreach).
- Success measure: significant reduction in treatment deserts and narrowing of rural-urban health disparities.
Sustainability Plan
- Ownership: Platform resides fully within state-controlled Google Cloud environments, ensuring control of data.
- Capacity Building: Analysts receive training and documentation to independently manage and extend the platform.
- Reusable Infrastructure: Designed as a backbone that can expand into multiple public health programs with limited incremental cost.
- Shared Financing: Modular structure allows for cross-agency cost sharing, aligning with CMS funding mechanisms.
Why Google Public Sector + Syntasa
- Proven Success: Projects across Arizona, Georgia, and Oklahoma show rapid deployment and measurable results.
- Pre-Built Accelerators: Tailored health analytics frameworks for chronic disease, opioid treatment, and behavioral health shorten implementation timelines.
- Unique Insights: Combines traditional health data with digital behavior signals for forward-looking, proactive insights.
- Scalability: Platform is cloud-native, highly secure, and flexible for multiple states.
Conclusion
Our AI-enabled Rural Health Resource Platform offers a practical and future-ready way to help rural hospitals and providers bring high-quality care closer to where patients live. By combining data integration, predictive analytics, and consumer-facing technology, the proposed solution ensures that rural communities are better supported, patients have faster access to care, and state leaders gain actionable insights for long-term transformation.
Google Public Sector and Syntasa stand ready to collaborate with policymakers and stakeholders under the OBBA framework to make this vision a reality.
Proposal 3
Introduction
Rural communities nationwide face enduring health disparities resulting from limited healthcare access, chronic disease prevalence, and provider shortages. These challenges contribute to worse health outcomes for rural residents, demanding innovative, data-driven approaches to remedy them.
Syntasa proposes a comprehensive Rural Health Provider Analytics (RHPA) solution leveraging Google Cloud’s advanced analytics technologies to integrate clinical, demographic, behavioral, and geographic data. This platform enables actionable insights to guide targeted interventions, optimize resource allocation, and ultimately improve rural health outcomes measurable at state and community levels.
Proposed Initiative
This initiative centers on enhancing chronic disease management and prevention by delivering a data-rich environment that identifies care gaps, tracks health outcomes, and empowers data-informed decision-making.
Key Components Include:
- Mapping Treatment Deserts: Visual heatmaps highlight rural areas lacking adequate healthcare services, facilitating focused intervention planning.
- Outcome-Based AI Recommendations: AI-powered reports identify high-impact strategies tailored to community-specific health profiles.
- Provider Impact Index: Links funding with health outcomes to quantify and prioritize resource allocation based on demonstrated effectiveness.
- Stakeholder Dashboards: Interactive dashboards provide real-time monitoring for providers, policymakers, and public health officials to collaboratively improve care delivery.
Potential Impact on Rural Healthcare
By integrating diverse datasets, RHPA supports evidence-based improvements in chronic disease prevention and management in rural communities. The platform’s insights enable states to prioritize interventions that yield measurable health improvements, reducing preventable morbidity and mortality while maximizing the efficient use of funding.
Plan for Implementation
- Discovery and Stakeholder Engagement: Collaborate with state agencies and healthcare partners to refine outcome metrics, validate data sources, and align with policy goals.
- Data Integration and Quality Assurance: Aggregate data from Medicaid claims, public health registries, provider networks, surveys, and digital behavior sources, ensuring data integrity and privacy compliance.
- Platform Deployment and Visualization: Deploy the analytics platform on Google Cloud, developing customized dashboards focused on outcome metrics and provider performance.
- AI-Driven Insights and Reporting: Generate dynamic reports recommending evidence-based interventions for chronic disease management.
- Training and Continuous Improvement: Equip stakeholders with training and support, incorporating feedback to optimize tools and analytics over time.
Preliminary Timeline and Milestones
| Phase | Discovery | Platform Deployment | Data Integration | Analytics & Dashboards | Testing & Delivery |
| Duration | Weeks 1-2 | Weeks 2-3 | Weeks 3-6 | Weeks 7-10 | Weeks 11-12 |
| Key Milestones | Kick-off meeting; Data source access confirmed. | Cloud environment provisioned; platform configured. | Data gathered, cleaned, and linked to locations. | Dashboards design and AI report generation finalized. | UAT complete; Final deliverables handed over |
Alignment with Cicero Institute Priorities
This proposal directly supports the Cicero Institute’s focus on innovative, evidence-based interventions improving rural health outcomes. By offering actionable analytics and AI-powered guidance, the RHPA platform enables sustainable transformation that is aligned with the Rural Health Transformation Fund objectives for measurable and lasting improvements in rural community health.
RadleyCare
Contact: Anson Frericks, CEO, [email protected]
Executive Summary
RadleyCare is addressing the acute BH workforce crisis by becoming the largest peer and family support employer for people with serious mental illness (SMI) within a year, using our innovative “Uber” and “Match.com” approach to developing and deploying mental health peer support.
RadleyCare is welcomed by local FQHC, CMHC, and safety-net hospital care teams as “amplifiers of care,” reinforcing existing treatment plans and reducing fragmentation.
RadleyCare is applauded by payers for utilizing measurement-based care for accountable and efficient service delivery.
RadleyCare is recognized by policymakers as aligning value across payers, communities, providers, and families through serving the most complex and expensive members (those with SMI) with the lowest cost care.
How we align/What we will produce
- Improved Health Care Outcomes: Peer support enhances access to preventive health services by addressing critical relational and navigational barriers to maintaining health, and RadleyCare’s peer program has rapidly expanded statewide in Ohio’s rural communities, providing flexible employment and driving evidence-based, outcome-focused interventions and comprehensive measurement-based care tools to improve disease prevention, chronic disease management, and behavioral health outcomes.
- Sustainable Access in Rural Communities: RadleyCare connects components of the behavioral health system, including primary care (FQHC), community behavioral health centers, rehabilitation, and acute providers—by amplifying a single unified, provider-developed treatment plan focused on functional gains to assist individuals in returning to work, school, and community life.
- Rural Behavioral Health Workforce Development: RadleyCare addresses the behavioral health workforce shortage by providing flexible jobs to trained peer supporters who are currently unemployed (e.g., over 3,000 in Ohio). Additionally, adding peer support to existing clinical teams enables providers to work at the top of their license and helps teams function at full capacity.
- Accountable Innovative Care for Rural Residents with SMI: RadleyCare delivers cost-effective, in-person and tech-enabled care for high-need community members, regularly reporting members’ progress, through evidence-based measurement tools, to ensure transparency and shared accountability.
- Tech Innovation to Improve Service Delivery: RadleyCare’s AI-driven integrated records and communications are designed to address key barriers to care, such as access—providing care when and where it is needed; accountability—offering measurement-based documentation and reporting tools; and coordination—facilitating real-time communication and operational integration with the clinical care team.
Our request for the RHT funds in Ohio
- Support the provision of peer support services reimbursed at Medicaid rates for all eligible individuals, irrespective of payer. Over a three-year period, supporting contracting and infrastructure will be developed, followed by a transition to value-based care across the multiple payers.
- Ohio Deliverables: Deploy 2,000 peers in rural Ohio (4,000 statewide) to serve 50,000 Ohio residents at the lowest cost of care (peer support rate) and reduce overall health spending.
Our request for the RHT funds in other states
- Ensure Peer support is a covered Medicaid service for persons with Serious Mental Illness (SMI), with rates similar to Ohio, to ensure the reimbursements are sufficient to cover cost of providing care.
- Support the provision of peer support services reimbursed at Medicaid rates for all eligible individuals, irrespective of payer. Over a three-year period, supporting contracting and infrastructure will be developed, followed by a transition to value-based care across the multiple payers.
VSee
Contact: Milton Chen, VSee CEO, [email protected], (650) 400-1798
Executive Summary
VSee proposes a modular, market-ready digital health platform that rural hospitals and clinics can deploy in weeks—not years—to expand access, improve outcomes, and lower total cost of care. The AI Command Center coordinates inpatient and outpatient tele-specialty care, remote patient monitoring (RPM), hospital-at-home (HaH), mobile clinics, and autonomous AI robots over a secure, interoperable cloud. The approach is evidence-based, fiscally accountable, and designed for replication across rural markets.
What the Platform Does
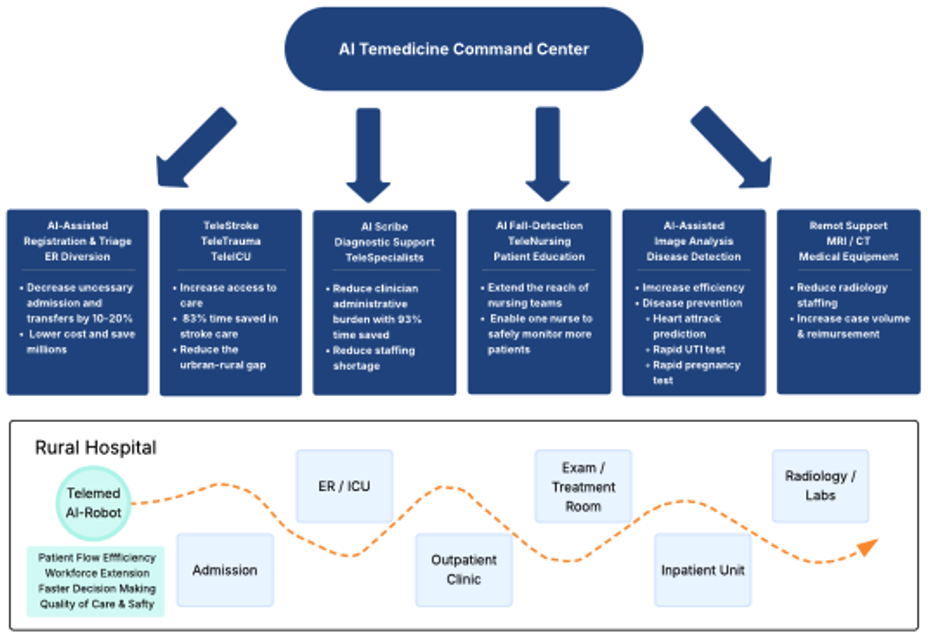
- AI Command Center: A set of tools to orchestrate eConsults, on-demand inpatient tele-specialty gaps (e.g., neurology, cardiology, psychiatry, radiology, infectious disease), direct admissions from virtual visits, and post-discharge automation. Includes tools for AI documentation, AI pre-diagnoses for stroke care, predictive analysis for high-risk patient heart attacks, and AI risk flags to increase physician throughput and reduce administrative burdens.
- Clinical applications and medical devices: Built on a digital health infrastructure with telehealth-integrated workflows (intake, consent, eRx, labs, billing, notes), agnostic medical device integration for RPM and hospital-at-home pathways, as well a mobile kits with satellite/broadband failover for disaster response and austere locations.
- Autonomous AI Robots with the ability to conduct check-ins, assign and lead patients to an exam room, discharge, assist in virtual rounding, and patient monitoring – freeing up staff time to provide better bedside care.
- Interoperability layer: Secure bi-directional exchange with Epic/Cerner/Meditech/HIEs (orders, notes, labs, discharge summaries, order-set transfer) via HL7 v2/FHIR/APIs.
OBBBA Alignment (categories addressed)
- Improve Access: Same/next-day virtual specialty access; tele-triage and hospital-at-home to keep patients local; rural hubs in retail clinics, schools, community centers, and public facilities
- Improve Outcomes: Faster specialist time-to-answer, automated 7-day follow-ups, RPM alerts for early intervention, and reduced re-visits and readmissions.
- Prioritize Prevention/chronic disease: RPM/RTM for CHF, COPD, diabetes, and hypertension; AI-supported self-management and care plan adherence.
- Strengthen Partnerships: A shared virtual specialty network linking rural hospitals, CAHs, FQHCs, EMS, and tertiary centers; standardized playbooks and quality dashboards to spread best practices.
- Enhance Workforce Supply: Tele-precepting, train-the-trainer programs, and AI documentation assist to reduce burnout and extend clinician reach.
- Data- and technology-driven care close to home: Interoperable, telehealth-integrated workflows minimize transfers and duplicate documentation.
- Long-term financial solvency: Reduce leakage and costly transfers; enable reimbursable telehealth, RPM/RTM/CCM, and bundled/episode strategies; lower fixed-cost pressure via shared services.
- Identify causes of rural risk: Low volumes, staffing shortages, transfer leakage, fragmented IT, and compliance overhead. The platform directly mitigates each by pooling demand, sharing specialists, and eliminating data silos.
- Other: Disaster-ready continuity when local IT is compromised; rapid deployment, failover device in austere settings.
Evidence and Precedents
- Interoperability at scale: Integration with Cerner drove an 88% increase in virtual visit completion for DaVita Kidney Care, improving coordination and documentation speed.
- Rapid deployment: VSee configured a disaster response EHR for a hospital in 2 weeks when the incumbent EMR was inaccessible—demonstrating speed and adaptability.
- Crisis resilience and measurable impact: In a cyberattack response, VSee-enabled teams restored radiology specialty access, processed 250+ radiology studies, and achieved sub‑hour emergency read times, maintaining patient flow despite core IT disruption.
- Enterprise security and trust: FedRAMP authorized, HIPAA and SOC 2 controls, and usage by federal agencies and NASA programs underscore security and reliability
- Implementation blueprint (actionable, replicable)
- Phase 0 (0–8 weeks): Governance setup (state PMO), site selection, data-use agreements, interface mapping; baseline metrics. Deliverables: charter, architecture, scorecard.
- Phase 1 MVP (Months 3–4): Go-live at 3–5 rural sites with inpatient tele-specialty and post-discharge automation; initial dashboards. VSee’s standard plan targets MVP within 3–4 months with UAT and soft launch [2].
- Phase 2 Scale (Months 5–8): Add outpatient telehealth, RPM, hospital-at-home; replicate build across regions; cohort enrollment and quarterly outcomes reporting. Once templates are set, site duplication typically compresses to days [2].
- Phase 3 Expansion (Months 9–12): Statewide rollout, public health automation, workforce tele-precepting, continuous optimization.
- Sustainability and market-based financing
- Leverage existing reimbursement: Telehealth parity, RPM/RTM, TCM/CCM, originating site fees; targeted episode/shared-savings pilots with Medicaid MCOs for CHF/COPD/diabetes and sepsis/ID pathways.
- Shared services model: Regional pooling of specialists and AI-enabled operations spreads fixed costs and stabilizes small facilities.
- Transparency and accountability: Performance-based disbursements tied to milestones and published dashboards (access, quality, cost).
Core Use Cases
- Inpatient telehealth: ED and inpatient access to specialists; tele-rounding; exchange and documented notes back to the host EMR.
- Telenursing (inpatient): 24/7 patient monitoring with AI enhancements, e.g., virtual fencing and predictive AI for fall detection, deterioration, organ failure, IV empty, etc.
- Outpatient telehealth and second opinions: eConsults (asynchronous), school-based care, mobile units, scheduled visits, direct admits when indicated; automated discharge follow-up.
- RPM and hospital-at-home: Vital device kits, AI risk flags, escalation protocols; safe step-down and recovery at home.
- Remote medical equipment operation: Access to remote biotechnicians to maximize use of advanced equipment (MRI, CT, ultrasound, etc.) with remote operation and support.
Accountability and Metrics
- Access: Median time to specialist consult; telehealth completion rate, transfer rate.
- Utilization/cost: 30‑day readmissions (RPM cohorts), avoidable ED visits, and length of stay.
- Continuity/quality: 7‑day post-discharge follow-up, infection-reporting timeliness/completeness.
- Workforce efficiency: Documentation time per visit (AI-assisted), provider satisfaction/retention.
- Implementation health: Sites live on time; contract‑to‑go‑live cycle; interface uptime.
- Quarterly dashboards are generated by the Command Center and shared with state HHS and Medicaid.
Risk Management
- Connectivity: Satellite/broadband failover, offline capture with deferred sync.
- Security: Role-based access, audit logging, continuous monitoring in a FedRAMP‑aligned cloud.
- Adoption: Train‑the‑trainer, tele‑precepting, and local champions at each site; user guides and remote learning.
Why VSee
- Rapid, configurable deployments and EMR interoperability at scale.
- Demonstrated outcome gains in integrated telehealth programs (+88% completion).
- Mission-ready resilience in crisis, with measurable clinical impact.
- Enterprise security and scalability trusted by federal and enterprise users.
Conclusion
Our proposal offers a practical, scalable path for any state to deploy a technology-first rural transformation—improving access and outcomes, strengthening financial viability, and building a durable, data-driven rural health infrastructure.
White-Label Telehealth Solutions
Chris Moose, [email protected]
Executive Summary
Rural hospitals are the backbone of healthcare access in their communities, yet they face severe financial strain, workforce shortages, and shrinking margins. Telehealth is the most obvious and impactful use of Rural Health Transformation Funds—but if deployed incorrectly, it could weaken rural hospitals by siphoning profitable services and eroding patient relationships.
A white-label telehealth solution, deployed under the brand of local hospitals, avoids these unintended consequences. It enhances access, strengthens finances, extends clinician capacity, and aligns with the “One Big Beautiful Bill’s” mandate for long-term systemic transformation—not just temporary fixes.
This change can be implemented quickly. Telehealth firms already offer white-label services to digital health organizations. Extending financial support for hospitals’ fixed costs to also adopt these solutions is an immediate, proven use of Rural Health Transformation Funds. By doing so, policymakers can accelerate deployment while ensuring the benefits accrue to local hospitals and communities, not outside vendors.
The Risk: Technology’s Unintended Consequences
History warns us that even beneficial technology can undermine critical institutions:
- The internet revolutionized information access but drew advertising revenue away from local newspapers. Journalism was left hollowed out, despite society’s continued need for robust reporting.
- Healthcare faces a parallel risk. Telehealth could siphon off high-margin, low-acuity visits, leaving rural hospitals with costly, less profitable services—and threatening their financial viability.
A white-label telehealth approach ensures that technology strengthens, rather than weakens, local institutions.
Why White-Label Telehealth Strengthens Rural Hospitals
- Preserves Patient Trust and Relationships
- Services operate under the local hospital’s name, not a distant corporate brand.
- Patients perceive continuity of care and loyalty to their community institution.
- Protects and Enhances Financial Viability
- Revenue from telehealth visits remains with the rural hospital.
- Profitable outpatient and chronic care services are not siphoned away by third-party telehealth companies.
- Delivers Cost Efficiency
- Shared technology infrastructure reduces overhead compared to each hospital building its own system.
- Compliance, IT, and integration costs are spread across multiple institutions.
- Provides Better Clinical Leverage
- Clinicians are a scarce resource, especially in rural areas.
- Telehealth enables a single clinician to serve multiple facilities, rather than being tied to one hospital.
- This model helps address clinician shortages by scaling expertise across communities while keeping local hospitals at the center of care.
- Keeps the Hospital Brand at the Forefront
- Patients associate their telehealth visits with the trusted local hospital.
- The hospital, not a third-party vendor, captures the clinical and financial value.
- Enhances Care Coordination
- Integration with the hospital’s records ensures telehealth visits complement in-person care.
- Prevents fragmentation and duplication of services.
- Ready to deploy and low-risk
- Telehealth is proven and rapidly scalable
- Enabling telehealth for Rural Hospitals is possible in the first months of funding
Broader Benefits Aligned with Rural Health Objectives
- Improved Access: Patients avoid long travel distances while still receiving care from their local hospital network.
- More Efficient Use of Clinicians: Scarce specialists can be pooled across facilities, reducing bottlenecks.
- Better Chronic Condition Management: Telehealth improves monitoring and follow-up for conditions like diabetes, COPD, and heart disease, lowering costly hospitalizations.
- Sustained Physical Infrastructure: Emergency, maternity, and surgical services—services that cannot be virtualized—remain financially viable when hospitals retain telehealth revenue streams.
Avoiding the “Temporary Fix” Trap
Rural Health Transformation Funds must not be spent on short-term, stand-alone telehealth vendors that weaken local systems. That would replicate the internet-advertising analogy: convenience today, systemic decline tomorrow.
White-label telehealth represents a durable capacity-building investment:
- It empowers rural hospitals to deliver digital care within their own ecosystem.
- It builds long-term financial resilience by reinforcing—not bypassing—local providers.
- It positions technology as a force multiplier for clinician capacity and patient access.
Alignment with the “One Big Beautiful Bill”
- The guiding principle of the One Big Beautiful Bill is long-term systemic change, not temporary solutions. White-label telehealth directly advances this mandate:
- Enhances the financial stability of rural hospitals, ensuring they remain viable community anchors.
- Addresses clinician shortages by enabling scalable use of limited talent.
- Improves patient outcomes through coordinated, accessible, and continuous care.
- Delivers cost savings while keeping critical physical healthcare infrastructure intact.
Conclusion
Telehealth is the obvious use of Rural Health Transformation Funds—but not all telehealth is created equal. Without careful deployment, it risks hollowing out rural hospitals in the same way the internet hollowed out journalism.
A white-label telehealth solution avoids that fate. It keeps patient trust and revenue within rural hospitals, leverages scarce clinician resources across multiple facilities, and sustains the financial base required to maintain emergency and inpatient services. Most importantly, it delivers long-term transformation consistent with federal policy objectives.
By choosing white-label telehealth, we ensure that technology strengthens rural healthcare rather than weakening it. This is not a stopgap. It is a proven, quick, and strategic investment in the resilience, vitality, and future of rural health.

Stay Informed
Sign up to receive updates about our fight for policies at the state level that restore liberty through transparency and accountability in American governance.
