
Making Sense of Harm Reduction:
An Analysis of the Impact of Substance Abuse on Public Health and the Evidence-Basis of Harm Reduction Practices
More people die of drug overdoses in the United States than anywhere else in the world.1
For the first time, the number of overdose deaths in the U.S. topped 100,000 in 2021, up 92.3 percent since 2015.2 In particular, deaths among young people aged 10–19 more than doubled between 2019 and 2021, with fentanyl accounting for 84 percent of those deaths.3 Drug use drives other pressing societal ills like crime and homelessness, and an estimated 85 percent of people in prison are addicted to drugs or alcohol.4 The most extensive study of American homelessness to date, Kushel and Moore (2023), found that about one in three people living on the street use methamphetamines, and another 14 percent use cocaine or opioids.5
Communities are desperate for solutions. In the haste for answers, a growing number of advocates have called for greater adoption of a set of practices known as “harm reduction” to help curb some of the negative consequences of drug use.6 Harm reduction is a philosophical reorientation of treatments and services that focuses on offering whatever limited care a client will accept rather than advocating for the more serious interventions they may need—including a client’s abstinence from drugs.7 Simply put, harm reduction orients the role of the provider around reducing the negative consequences of actions rather than trying to change individual decision-making. For example, a client may refuse to stop using drugs but may accept clean needles, which reduces the likelihood of spreading bloodborne diseases such as HIV and hepatitis C.
However, it is imperative that policymakers tread carefully when considering harm reduction as opposed to other drug intervention programs. The stakes are high, and the available evidence in support of harm reduction varies in both quantity and quality. Moreover, harm reduction encompasses a diverse category of practices, some of which are more supported by evidence than others. Given the high-risk factors of the drug-using population, policymakers must take great care to avoid implementing policies intending to help that could have devastating unintended consequences.
The following report summarizes the complexities of substance abuse and the various responses categorized as “harm reduction.” We intend this to be a reference guide for policymakers and service providers. The report begins with an overview of the significant public health concerns regarding substance abuse, categorizes and explains the different types of harm reduction practices, then summarizes recent studies on their effectiveness.
Section I: Public Health and Substance Abuse
Drug users experience a wide range of serious health challenges both as a direct result of the consumption of drugs and the risky behaviors associated with drug use. Harm reduction aims to reduce the prevalence of disease and certain types of mortality by mitigating the risk behaviors most closely associated with specific negative health effects while not necessarily stopping the drug use itself.
It is important to note that types of drugs or routes of administration (ROA) vary in their risks of disease and mortality. Generally, injection drug use carries the highest risk of disease, and opioids have the highest risk of mortality. Even so, the risks and benefits of each type of drug and route of administration are not always aligned. For example, a study of smoking heroin-laced cannabis and injecting heroin found that while smoking had lower risks of HIV, it carried significantly higher rates of relapse after treatment.8 It is important to investigate the implications of both the method by which drugs are consumed and the effects of the drugs themselves.
Health Risks by Method of Drug Consumption
The four significant modes of drug use are oral, injection, inhalation, and intranasal consumption. While specific drugs are associated with certain types of consumption, geography is also associated with different modes of drug use. For example, people living in rural areas and western states are much more likely to inject drugs than those in urban areas and northeastern states.9
Oral
Oral consumption of drugs is, broadly speaking, the most common route of administration by volume, especially among urban populations and for consumption of illegal prescription opioids.10 Potency and health risks that result from oral consumption vary by drug. Oral consumption of cocaine is comparably potent to intranasal consumption, but both methods are about one-fourth as powerful as smoking and one-eighth as potent as injection.11 Opiates (such as heroin and morphine that are derived from natural sources) and opioids (synthetic drugs) are less potent when consumed orally than by other routes of administration because of initial metabolism in the liver, but this can, in turn, lead to more direct liver damage than consumption via different routes of administration.12 Liver damage and failure are the primary direct health risks of this route of administration.
Injection
Approximately 3.6 million American adults inject drugs, with non-Hispanic white men aged 18–39 being the most frequent users.13 However, most drug users do not inject drugs.14 Heroin users have the highest proportion of users who inject at a rate of 41 percent, while fewer than 10 percent of methamphetamine, cocaine, and users of other stimulants will consume drugs through injection.15 A study based on the National Survey on Drug Use and Health found that while people who inject drugs tend to be in poorer health and more dependent on substances than drug users who do not inject, they are also four times as likely to receive treatment.16
The three major disease risk factors for people who inject drugs are HIV, HCV (hepatitis C virus), and skin infections. While approximately 1.2 million people in the U.S. have HIV (about 32,100 new infections each year), the vast majority of new infections (92 percent) are the result of sexual contact.17 The total number of new HIV infections resulting from injection drug use is relatively small: only 2,500 (eight percent) of new HIV infections.18 This number has remained consistent, increasing by only four percent since 2017.19 Treatment for HIV is costly, at approximately $36,000 per year.20
Hepatitis C, on the other hand, is far more prevalent among people who inject drugs, which is the largest group infected with HCV.21 Annually, there are more than 100,000 new cases of hepatitis C. Among long-term drug users who have injected drugs for at least 10 years, rates of HCV are as high as 70–90 percent.22 Among young, relatively new users, HCV incidence is estimated at 8–25 percent per year, and the National Institute of Health estimates that a quarter of new intravenous drug users typically contract HCV within two years.23 The only treatment is an expensive regime of drugs that costs upwards of $23,000 per month for a course of treatment lasting 12–72 weeks.
Skin infections are also disproportionately associated with those who inject drugs. Each year, there are an estimated 155,000–540,000 skin infections among people who inject drugs.24 One study found that about 39 percent of people who inject fentanyl reported a skin infection over a three-month period.25 A conservative estimate puts people who inject drugs are about 10 times more likely to contract skin infections than the general population, though the actual risk may be much higher because the sample likely consists of a younger age distribution than the general population, and older people are more apt to report skin infections.26
Inhalation
Inhaling drugs is generally considered to have fewer risks than injecting, though it still carries many serious health risks. At a basic level, inhaling drugs, such as through smoking, damages the respiratory system and can cause long-term health complications ranging from asthma to lung cancer.27 Smoking methamphetamine, crack cocaine, or heroin are all associated with increased risk of lung infections like pneumonia.28 Smoking methamphetamine is also associated with severe dental disease.29–30
Studies comparing people who inhale drugs, inject drugs, and those who do both offer greater nuance regarding the relative risk of inhalation. One study of methamphetamine users found that those who only smoke have very similar outcomes in terms of the amount of drugs consumed, frequency of use, episodes of violent behavior, and likelihood to commit crime as users who only take drugs by injection.31 Another study comparing the two concluded that people who smoke methamphetamine had more intense use patterns than people who inject methamphetamine and otherwise had similar levels of psychological distress, poor physical and mental health, and criminal involvement.32
These findings differ slightly depending on the drug in focus. While intravenous fentanyl users had statistically similar utilization of emergency services as fentanyl users who smoke, users who inject carried a 40 percent higher risk of non-fatal overdose and a 235 percent higher likelihood of skin infection compared to those in the smoking group.33
The available evidence confirms that while inhaling drugs carries many risks, it is generally less dangerous than injecting drugs.
Intranasal
The third primary way of using drugs is intranasally snorting the substance directly into the nose. Heroin, methamphetamine, cocaine, and many other substances are taken this way. Generally, snorting drugs carries less stigma than injecting and, in some cases, smoking them. It also tends to have a lower risk of disease.
Even so, snorting any drug will damage nasal tissues, create sores and holes in the nose and nasal septum, and damage the palate.34 Snorting some drugs carries even greater risks than those. For example, snorting methamphetamine often leads to a less intense high, which causes people to use it at a greater frequency than they might with other modes of ingestion.35 Continued use by snorting, like smoking or injecting, results in severe damage to the nervous, respiratory, and renal systems.36
Some studies have found differences in treatment outcomes for individuals who use drugs intranasally compared to those who primarily use through other modes. One study of cocaine users found that the intranasal users stayed in treatment longer and had a greater number of maximum days abstinent compared to people who smoked cocaine.37 However, other outcomes were virtually the same for both groups.
Mortality and Substance Abuse
Death is distinct from other public health issues related to drug use. While infectious diseases, cancer, and strained organs and veins pose significant health risks, including death, they typically develop with continued drug use over time. But over the past few decades, death by overdose—which can occur in a single use with immediate effect—has become the leading public health issue among people who use drugs.38
In the last year, approximately 9.2 million Americans misused opioids—of which 1.1 million used heroin.39 Another estimated 2.5 million people reported using methamphetamine, and 996,000 people used crack cocaine.40-41 Of those who used any type of drugs, 106,000 died from a drug-involved overdose.42 More than twice as many people died from overdoses of synthetic, non-prescription opioids—namely fentanyl—than from stimulants like cocaine and methamphetamine. Of deaths resulting from cocaine or methamphetamine overdose, a sizable majority also involved opioids.43
Drug use has become more dangerous than it was in the past in large part because of the prevalence of potent opioids like fentanyl and similar substances. In the case of methamphetamine, overdose deaths between 2015 and 2019 increased by 180 percent, while the number of users over that same period increased by only 43 percent.44 When overdose deaths are sorted by both drug type and the presence of other substances, a clearer picture emerges. The number of overdose deaths associated with a mixture of methamphetamine and opioids increased by 266 percent between 2015 and 2019 and represented 54 percent of all methamphetamine-related deaths.45 Overdoses involving mixtures of methamphetamine with other potent drugs like cocaine also saw considerable growth—379 percent—but represented a much smaller proportion of total deaths at 11 percent.46 In comparison, the number of deaths associated with methamphetamine overdose without opioids or cocaine increased by 115 percent over the same period.
Another factor that contributes to the deadliness of drug use is environmental—whether someone uses drugs alone. A study of opioid deaths in New York City found that three-quarters occurred in private homes, where individuals are more likely to use drugs alone.47 Other studies have found a similar proportion of drug-related deaths occurred while a person used drugs alone.48
Causes of Death by Type of Drug
The leading causes of death for people who use drugs vary to some degree by what type of drug the individual primarily uses. The two leading narcotic drugs used in the United States that result in death are methamphetamine and those in the broad category of opioids.49
Methamphetamine
People who use methamphetamine are an estimated six times more likely to die prematurely than the general population when adjusted for age.50 There is not one clear leading cause of death for methamphetamine users, and it is not entirely clear what drives the different outcomes of mortality studies. The leading causes of death in one study were suicide (32 percent of deaths) and accidents (20 percent), with only three percent the result of overdose and no deaths due to HIV. Another study of methamphetamine users in California found that cardiovascular disease, HIV, cancer, and drug overdoses were the leading causes of death.51 While intentional suicide was not a leading cause of death, approximately half of methamphetamine users who died over the course of the study had attempted suicide.
Opioids
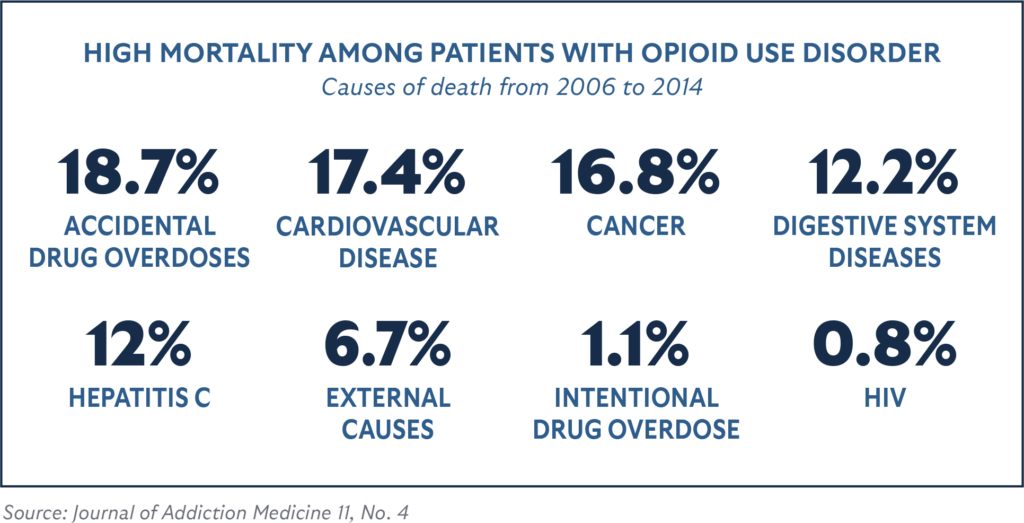
People who use opioids without treatment are estimated to have a mortality risk that is six times higher than the general public.52 A meta-analysis of 58 studies of opioid-dependent individuals found that overdoses were the most common cause of death.53 Another study of mortality risks found that approximately 18.7 percent of deaths were related to accidental drug overdoses, followed by 17.4 percent from cardiovascular disease, 16.8 percent from cancer, 12.2 percent from digestive system diseases, 12 percent from hepatitis C, 6.7 percent from external causes (such as accidents or violence), 1.1 percent from intentional drug overdose, and 0.8 percent from HIV.54 A 17-year cohort study had similar findings, with 33.1 percent dying from overdoses and 9.6 percent from digestive system diseases, while also finding that 5.2 percent died of lung disease and 4.9 percent from suicide.55 In general, mortality risks from the effects of drugs are far higher than the risks posed by infectious diseases associated with using drugs. For example, the age-adjusted death risk factor of hepatitis C is seven times smaller than that of death from drug overdose.56 Mortality risks do improve dramatically for people who stop using drugs, even if they used drugs for an extended period before stopping. In a study of people who used opioids daily over a 10-year period, those who stopped using had a 45 percent lower risk of death compared to those who continued daily use.57 However, risks remain higher for all opioid users even after quitting when compared to those who never used drugs. Compared to the general population, mortality risks remained many times higher for all current and former opioid users.
Section II: Types of Harm Reduction
- Harm reduction as a category covers a wide range of practices. The most common categories of harm reduction include:
- Information, education, and counseling
- Fentanyl test strips
- Naloxone (commonly known as the brand name Narcan)
- Good Samaritan protections
- Overdose hotlines
- Needle and syringe exchange programs
- Medication-assisted treatment
- Supervised injection facilities
Information, Education, and Counseling offer the public education that covers the risks of drug use while also providing practical information to reduce the risks of addiction, disease, and death if they do choose to use drugs. One example is a high school curriculum called “Safety First,” developed by Drug Policy Alliance and Stanford University’s REACH Lab.58
Fentanyl Test Strips are treated paper strips that can detect the presence of fentanyl in other types of drugs, such as heroin, methamphetamine, and cocaine. These strips inform people when their drugs are likely to be contaminated with fentanyl, though they do not provide information about how much fentanyl is present beyond the threshold of detection.
Naloxone is a medicine, also known by the brand name Narcan, that can be administered to someone who has overdosed on opioids to reverse the effects of the overdose and prevent death. An example of policies that promote this is Vermont’s community-based distribution of Narcan.59
Good Samaritan Protections are laws that protect people from prosecution for certain drug-related crimes if they call emergency services to assist someone who has overdosed. An example of this type of policy is New York’s 911 Good Samaritan Law.60
Overdose Hotlines are services that encourage people who use drugs to call a hotline that records the information required to summon emergency services if an overdose should occur. The caller uses drugs while on the phone with a hotline operator, who will then call emergency services if they are disconnected or the caller is unresponsive. An example of this service is the Never Use Alone hotline.61
Needle and Syringe Exchange Programs offer people who inject drugs access to clean, sterile syringes and needles so they do not reuse or share needles that could be contaminated with infectious diseases. Some programs require a one-to-one exchange in which an individual must trade a used needle to get a clean needle in exchange, while others allow individuals to take a certain number of clean needles without a trade-in. An example of this program is Florida’s Infectious Disease Elimination Act (IDEA) needle exchange sites.62
Medication-Assisted Treatment, also known as Opioid Substitution Treatment and pharmacotherapy, prescribes opioid-dependent intravenous drug users with long-acting opioid agonist medications. The most common opioids prescribed for this are methadone and buprenorphine, Suboxone, and occasionally naltrexone. These opioids are taken orally rather than injected, and they are less potent and less likely to be contaminated than illegally obtained opioids. An example of this is Palm Beach County, Florida’s Medication-Assisted Detox Treatment Program.63
Peer and Supervised Injection Facilities are facilities where drug users may inject illicit drugs in a hygienic environment or seek assistance in injecting drugs from a peer, without the threat of prosecution, and in proximity to medical professionals who can administer naloxone in case of an overdose. The only example of this type of site in the United States is OnPoint NYC.64
Section III: Effectiveness of Types of Harm Reduction
Evaluating the effectiveness of harm reduction as a category is extremely difficult because of the wide variety of methods used in different harm reduction practices. Instead, it is more useful to evaluate the effectiveness of each practice individually, which offers a more nuanced understanding of the extent to which discrete harm reduction practices could be adopted as meaningful solutions by policymakers and service providers. It is worth noting not all harm reduction practices have received equal attention from researchers, so the evidence base varies considerably depending on the practice.
Information, Education, and Counseling
Information, education, and counseling could be considered the most basic forms of harm reduction. These practices are limited to providing people who may or may not use drugs with clear, practical guidance on the specific risks of certain types of drugs and methods of drug use. There are three primary venues for the most direct versions of this practice: online, in community centers, and in schools and colleges. More passive versions include advertisements on billboards, public transportation, and through digital, radio, and television channels. There do not appear to be any studies that evaluate the comparative effectiveness of each method of instruction, and most evaluations focus on school-based programs. One pilot study of a program in Australia found a significant increase in drug literacy levels and practical ways to minimize certain dangers associated with using drugs after being exposed to the program.65 The study did not provide measures of impact on actual behavior or longitudinal outcomes in terms of drug use, crime, disease transmission, or overdose. It also did not measure whether students would be more or less likely to use drugs after taking the course. A recent study of a U.S. program, Safety First: Real Drug Education for Teens, found its material increased student awareness of drug related knowledge, but more importantly, students also reported being less likely to use drugs.66 Those who did use drugs did so at lower levels than other students.
While the available studies acknowledge the need for further research into the effectiveness of these programs, their early results are promising for policymakers and educators.
Fentanyl Test Strips
Fentanyl test strips cost approximately one dollar per single-use test strip. They are 96-100 percent accurate and can detect more than 10 different variants of fentanyl.67 User error, however, can result in false or inaccurate results. Other limitations include the presence of fentanyl at levels below the detection threshold and the inability to measure specific amounts of fentanyl in a sample. Fentanyl test strips are also limited because they do not test for other potential contaminants that could present different but similarly harmful effects, thus giving users a false sense of security. Other issues raised by researchers include the potential risk for people to grow increasingly complacent if they use drugs after receiving positive test results without an overdose.68
Studies of the impact of fentanyl test strips have found them to be generally effective. A 2019 study by RTI International found that, of those who used test strips, 43 percent reported a change in how they use drugs, and 77 percent reported feeling safer than when they used drugs without test strips.69 Participants reported a variety of specific changes to their drug use behavior, including 32 percent who used a smaller dose of the drug. Another study in Vancouver found that drug users who received a positive result from their test strip were 10 times more likely to reduce the dose they consumed, which resulted in a 25 percent reduction in their chances of overdose.70
Another study investigated how people who use drugs perceived testing information. The study found that 73 percent of drug users had a moderate to high interest in knowing if there is fentanyl in their drugs before using, and 70 percent reported that knowing if fentanyl was present would impact how they use their drugs.71 While fentanyl test strips have quite favorable studies supporting their use, 32 states have legal barriers that prevent widespread adoption of fentanyl test strips, which can be considered drug paraphernalia under certain definitions.72 Three of those states do specifically permit fentanyl test strips when they are used at harm reduction centers. Currently, at least 10 states have pending bills that would exclude fentanyl test strips from their legal definition of drug paraphernalia.
Naloxone
Naloxone has long been considered an effective way to counter an opioid overdose. Naloxone is injected into a person experiencing an opioid overdose to reverse its effects and prevent the person from dying. All 50 states and Washington, D.C. have some form of legal access to naloxone, though the specific rules vary considerably.73 An estimated 75–100 percent of those given naloxone during an overdose end up surviving.74 While naloxone has some negative effects, such as confusion, vomiting, seizures, and, in some cases, cardiac arrest, serious adverse effects are generally rare.75 Naloxone is a safe method for reversing opioid overdoses. More recently, Narcan, a name-brand naloxone nasal spray, has been approved as an over-the-counter opioid overdose treatment supplied to drug users, family members, and others who may be near drug users to jumpstart treatment before paramedics arrive. Narcan requires less training to use correctly than injectable forms of naloxone and is more widely available in many places, while legal barriers to accessing naloxone remain in some parts of the United States.
A systematic review of studies of the use of naloxone found strong evidence that bystanders of drug overdoses—who are typically also using drugs themselves—will utilize naloxone when it is available to them, and they know how to use it.76 The studies also found evidence that community overdose prevention programs are effective in training individuals to use naloxone.
One recent major study on the impact of expanding naloxone access, however, found some negative consequences. The study found that broadening naloxone access may have led to more people using opioids, fewer people seeking treatment, considerable increases in drug and property crime, and more overdose-related emergency room visits.77 The study did not find evidence that naloxone access led to a reduction in overdose deaths.
The available evidence suggests that naloxone is effective in saving individual lives in individual instances but that it is not itself a solution to the drug crisis at a societal scale. Policymakers should also be mindful that naloxone is not effective in reducing the portion of overdoses that are not related to opioids, which is smaller but growing at comparable rates.
Good Samaritan Protections
Some states and localities have created legal protections for so-called “Good Samaritans” who call emergency services for someone who is experiencing an overdose. These protections are designed to mitigate a bystander’s fear of criminal prosecution if they are also using drugs or have drugs in their possession. In 2021, the U.S. Government Accountability Office published a review of seventeen studies on the effectiveness of Good Samaritan protections and found that adoption of these laws is generally associated with lower rates of overdose deaths from opioids. However, the studies have many methodological limitations, and these laws merit further study. Additionally, there are limitations to the effectiveness of the laws themselves, such as the wide variability in the public’s knowledge of them.78 A comparative study of drug overdoses in New York and New Jersey found that New York’s adoption of Good Samaritan protections increased the utilization of emergency services for drug overdoses apart from the broader increase experienced in both jurisdictions.79 The study did not conclude whether the protections had a discernible effect on overdose deaths.
While there is favorable, but not necessarily rigorous, evidence in favor of Good Samaritan laws, no studies have shown negative outcomes. Most jurisdictions in the U.S. have Good Samaritan protections, with laws in effect in 47 states and Washington, D.C.80 Kansas, Texas, and Wyoming are the only states remaining without these protections in place.
Overdose Hotlines
Overdose hotlines are a form of supervised injection that aims to reach people who use drugs alone in private spaces. There are two major examples of this practice in North America: one in Canada and one in the United States. The Canadian program, known as the National Overdose Response Service, was piloted from December 2020 to February 2022.81 An estimated 50 to 70 percent of overdoses in Canada occur among people using drugs alone, which limits the ability of others to provide life-saving interventions.82 A study of the hotline pilot program found that, of 2,171 calls and 222 unique callers who used a range of drugs (cocaine, opioids, and methamphetamine) through a variety of methods (intravenously, smoking, and intranasally), there were 53 overdoses and no fatalities.83 In the United States, an estimated two-thirds of overdose deaths occur without a bystander.84 Although no independent studies have been conducted on the effectiveness of the hotline in the U.S., the Never Use Alone organization reports receiving 33,000 calls from 11,500 unique people, resulting in 110 overdose reversals.85
There are reports of the development of other forms of technology beyond traditional phone lines to serve a similar purpose, but there is limited information available about those services or devices.86
The limited evidence in support of overdose hotlines is a reason for prudence, but the practice does offer a less contentious alternative to supervised injection sites—and one that is legal.
Needle and Syringe Exchange Programs
Needle and syringe exchange programs are likely the most widely known of harm reduction practices. There are approximately 400 of these programs in the United States, with active programs in 43 states plus Washington, D.C. and Puerto Rico.87
There are three primary goals for these programs: first, to reduce infectious disease transmission; second, to reduce the volume of needles discarded in public; and third, to engage hard-to-reach individuals with services.
To achieve the first goal, needle and syringe exchange programs aim to provide sterile needles to people who might otherwise use potentially contaminated needles to inject drugs. According to a meta-analysis, needle and syringe programs are generally effective in reducing injecting risk behaviors, such as sharing or reusing needles or syringes.88–89
There is less evidence, however, that needle and syringe programs effectively reduce infectious disease transmission. The meta-analysis above found “tentative review level evidence” to support effectiveness in reducing HIV transmission but also reports that “overall, the primary studies with the most rigorous designs reported mixed findings with an equal number of cohort studies reporting positive, null and negative associations.”90 Two of the most rigorous reviews found conflicting results. Aspinall et al. (2014) found that individuals who participated in needle and syringe programs had a 34 percent risk reduction of HIV transmission compared to those who were never or less frequently exposed.91 The review also found, however, that studies focusing on groups post-1990 had lower impact estimates. Jones et al. (2008) found only tenuous evidence to support the effectiveness of needle and syringe programs on HIV risk among intravenous drug users.92 Though not named as a factor in these reviews, it is likely that high-risk sexual activity among people who inject drugs contributes to the limited effectiveness of needle and syringe exchange programs in reducing HIV transmission. A cursory look at HIV statistics shows that sexual transmission is by far the leading cause of new incidences of HIV.93
Needle and syringe programs appear to have limited effectiveness in reducing the spread of hepatitis C as well. The aforementioned reviews found insufficient evidence to determine whether these programs reduced hepatitis C transmission.94-95 One review included in Jones et al. did find enough evidence to make a conclusion about the impact of needle and syringe programs on hepatitis C infection. That review concluded that the impact is less than that the program has on HIV infection. Like HIV, high-risk sexual activity among drug users may also be a factor that makes it more challenging to measure the effectiveness of needle and syringe programs in reducing hepatitis C transmission.
One of the most notable studies of needle and syringe programs, from the National Bureau of Economic Research, found troubling evidence that while these programs may reduce local disease transmission, they are associated with considerable increases in drug-related crime (16 percent), overdose mortality (13-15 percent), and theft (24 percent).96 These outcomes justify a high degree of caution among policymakers who are considering needle and syringe programs for their communities.
There is some evidence that needle and syringe programs are successful in achieving their second goal: reducing the amount of publicly discarded needle and syringe waste. A study of harm reduction centers in Spain found that creating new needle and syringe programs was associated with a short-term increase in publicly discarded syringes, followed by a sustained decline that was geographically consistent.97 The study notes, however, that concurrent police interventions likely also contributed to the city-wide decline in syringe waste.
The third goal of needle and syringe programs is to engage hard-to-reach and treatment-resistant populations with services by building trust through syringe exchanges. There is limited evidence that needle and syringe programs do this successfully. One study found that consistent engagement with needle and syringe programs was associated either with increased treatment participation (in the unadjusted analysis) or with predictors of treatment participation (in the adjusted analysis).98 Anecdotally, many harm reduction practitioners claim service engagement—especially services short of treatment—is the most apparent benefit of needle and syringe programs, above even the first two goals related to disease prevention and waste mitigation. These services could range from wound care to food and financial benefits. Even so, it is likely that there are other ways beyond providing needles and syringes that could attract individuals to participate in services.
Policymakers and service providers should carefully weigh their options given the limited evidence that these programs are effective in achieving the primary and secondary goals as well as the possible tradeoffs in terms of crime and overdose mortality.
Medication-Assisted Treatment
Medication-assisted treatment, also known as opioid substitution treatment, is a program that discourages the injection of illegal opioids by decreasing their euphoric effects and the symptoms of withdrawal through alternative oral drugs like methadone and buprenorphine. A 2021 report by Pew found that restrictions on medication-assisted treatment vary widely by location, and 80 percent of counties across the country have no access to programs at all.99 Approximately 19 states and Washington, D.C. have barriers to opening new programs, hindering future growth.100 Studies estimate that only 13–20 percent of people with opioid use disorder have accessed medication-assisted treatment.101
There is strong evidence that medication-assisted treatment is effective, but it is by no means a cure-all. People who use opioids without treatment are estimated to have a mortality risk that is six times higher than the general public.102 A study of 32,322 opioid users in California found that of those who received methadone maintenance treatment, the mortality risk was less than half that figure, at a factor of 1.8.103 Other studies have found that people who receive medication-assisted treatment decreased their risk of premature mortality by 500 percent.104
The decrease in illicit drug use associated with medication-assisted treatment further reduces the risks associated with injecting drugs, such as disease transmission. There is strong evidence that people participating in medication-assisted treatment have lower risks of contracting an infectious disease like HIV.105
Even so, many people receiving treatment continue illicit opioid use in addition to receiving methadone. Patients on methadone had 33 percent fewer opioid-positive drug tests, but that means that 67 percent of those given the methadone prescription took this additional opioid along with those they use illicitly.106 Another study found about 25 percent of patients prescribed buprenorphine also tested positive for another illicit drug more than once within a year and had to be disqualified from the study.107
There is also some evidence of people who had not previously used opioids beginning their drug use through medication-assisted therapy, particularly in institutional settings like correctional facilities. In jails and prisons, non-prescribed buprenorphine is considered the most widely available opioid. Among recently incarcerated adults with opioid use disorder, 81 percent reported non–prescribed buprenorphine was “somewhat” or “very” easy to get, and 39 percent reported using non–prescribed buprenorphine while incarcerated.108 The most common motivation for the use of non-prescribed buprenorphine while incarcerated was “getting high/mood alteration,” whereas the motivation for non-prescribed buprenorphine outside of prison was more often therapeutic, such as self-treatment.109
Peer and Supervised Injection Facilities
Supervised injection facilities (SIF) are likely the most controversial harm reduction practice, as they most directly enable the underlying drug use behavior. These sites can utilize peers or service providers to oversee drug use or even directly assist in the consumption of drugs. Supervised injection facilities attract some of the highest-risk drug users. An estimated 40 percent of clients at a supervised injection facility in Montreal were daily users, and two out of three clients inject drugs at least once per week.110
Advocates of supervised injection sites claim no one has died of an overdose while using at one of these facilities.111 A recent systematic review of supervised injection facilities found strong evidence that safe injection facilities reduce both overdoses and overdose-related deaths in their vicinity, with net reductions in deaths as high as 26 percent.112 The review found limited evidence of supervised injection facilities modestly increasing the likelihood of their clients utilizing addiction treatment programs, with one robust study finding that SIF clients were 1.4 to 1.7 times as likely to enroll in treatment.113 In regards to crime, the review found compelling evidence of an “abrupt, persistent decrease in crime” in the area around a supervised injection site after one opened in Vancouver, Canada. There is less evidence in support of the effectiveness of safe injection facilities in reducing the transmission of infectious diseases among people who inject drugs. The aforementioned systematic review found no statistically significant impact in any quality studies.114 A meta-analysis found tentative evidence of effectiveness in reducing disease-related risk behaviors associated with injection, with one cross-sectional study finding a positive association and another finding non-significant difference in the use of sterile syringes and sharing of syringes or equipment among supervised injection facility clients compared to non-SIF clients.115 The one review that covered evidence of the impact of SIFs on HIV infections found no increase or decrease, though the authors note a low prevalence of HIV among those tested during the period of evaluation found other unexpected results. A 2020 study of a SIF with more than 5,600 visits found female clients were more than twice as likely to overdose at the facility than if they received no assistance, while men had no statistically significant difference.116 Out of 146 overdoses, however, there were no fatalities. Other unexpected findings were that women were far more likely than men to receive direct assistance in administering drugs, and people of both genders who received assistance with injecting fentanyl had higher odds of overdosing than those who injected fentanyl without assistance. Another 2020 study of a SIF in Canada found that male clients experienced less criminal violence than male non-clients, but there were no differences for women.117 These gender disparities raise important questions for policymakers and service providers.
Many researchers are critical of the quality of research currently available on SIFs, reporting that the lack of rigorous studies and the lack of tracking long-term outcomes make it impossible to draw substantial, reliable conclusions.118–119
Some people involved directly in supervised injection facilities also voice concerns. When the site manager of SIF Safepoint in Ontario, Canada was asked how many of its 800 drug-using clients entered treatment, he admitted it was “not many…I’d say a handful.”120 Other employees at these facilities have expressed skepticism anonymously about the effectiveness of their facilities, admitting that their work feels more like it is enabling drug abuse than contributing to a solution.121 Moreover, the cycle of drug use, overdose, and revivification is rarely enough to compel people who use drugs to change their behavior, with practitioners estimating this is the case in about one out of every 30 SIF overdoses.122 Previous drug users have also spoken out against SIFs, arguing that by making it so easy and safe to use drugs, SIFs implicitly endorse drug use.123
Other non-academic reports indicate that crime has increased near certain SIFs. As the number of client visits climbed rapidly at one SIF in Calgary, the number of social disorder calls and incidences of violent crime in a 500-meter radius of the premises far exceeded all-time highs.124 Police authorities have also found these sites to become hotspots for drug dealers.125
Overall, there is no compelling, consistent evidence in support of supervised injection facilities. Policymakers and service providers should be cautious about experimentation with these facilities. So far, there is only one supervised injection facility in the United States, though some cities are considering opening sites in the future.
Conclusion
The broad category of “Harm Reduction” includes many innovative responses to the worsening drug crisis in the United States. Some harm reduction practices hold promise as meaningful ways to save lives, but the variability in the amount and quality of evidence across harm reduction practices demands caution and prudence on the part of policymakers and service providers. Harm reduction is not an unequivocal good.
Based on the most pressing public health needs due to widespread substance abuse and the available evidence for the most common harm reduction practices, policymakers should focus their attention on the following: information, education, and counseling; fentanyl test strips; naloxone; Good Samaritan protections; and medication-assisted treatment. While the available evidence in support of overdose hotlines is limited, the potential impact and comparatively low risk of this practice merits further investigation by policymakers. However, policymakers and service providers should be very cautious of needle and syringe exchange programs and supervised injection sites, weighing the public health and public safety tradeoffs demonstrated by the available studies of those programs.
Most importantly, advocates, policy analysts, and researchers should support further, unbiased investigation of harm reduction programs and provide communities and policymakers with honest appraisals of the evidence currently available.

Stay Informed
Sign up to receive updates about our fight for policies at the state level that restore liberty through transparency and accountability in American governance.

