
Cutting the American Physician Shortage With International Doctors
Introduction
Regular doctor visits keep patients healthier and help patients identify health problems earlier and with a greater possibility for recovery.1 But regular visits to a healthcare professional are becoming more challenging because of a shortage of professionals able to treat patients. Even patients who understand the importance of a doctor visit may be unable to visit the doctor when they want to. So, the question for many Americans is not whether seeing a healthcare provider would be beneficial but rather whether they can find a healthcare provider who is able to provide them with care.
Unfortunately, too many conversations about access to care still center not around whether a patient can see a physician or healthcare professional but whether that patient has a third-party payor. For most of the last twenty years, the “access to healthcare” discussion has focused on whether the patient has health insurance coverage through an employer, the individual market, or a government program.2 But while being covered by health insurance is often an important proxy for whether the patient can afford an expensive treatment, insurance does not guarantee that a patient will be able to find a doctor in their moment of need.3 This focus on being “covered” with some kind of insurance product ignores the much more pressing question for millions of Americans: are there enough healthcare providers to meet patient demand?
While only a small portion of the U.S. population lacks access to health insurance, millions of Americans live in areas without adequate doctor supply, according to the Centers for Disease Control.4–5 State and local leaders nationwide recognize this challenge, but only a handful of states have taken significant steps to dramatically increase healthcare provider supply to meet these needs.
One relatively untapped potential source of medical talent is doctors currently licensed outside the United States. Thousands of workers living in America have healthcare expertise and training from abroad. Still, licensing rules prevent many of these workers from fully using their talents to treat patients.6 States should no longer leave that base of talent on the sidelines but should instead make sure those doctors have a pathway to serve patients in the United States. That pathway should allow an internationally licensed doctor to practice without repeating training she has already completed so that the newly licensed doctor can treat patients as soon as feasible.
Physician Shortage
Healthcare worker shortages made accessing healthcare services difficult before the Covid-19 pandemic.7 Increased healthcare demand and the challenges associated with the pandemic exacerbated the problem—and the crisis has worsened since. Many commentators and industry insiders expected a return to “normal,” however adequate access to healthcare is as far off as ever, with no end in sight for most Americans. This is largely due to the critical shortage of physicians, potentially exceeding 100,000 by 2034.8 The most significant contributors to the shortage include physician burnout, a growing population, a relatively static supply of medical training slots, and an aging population with ever-growing healthcare needs.9 Significant deficits in both primary care providers and specialists cause low appointment availability, increasing costs, and poorer health outcomes.10,11,12

Current and Projected Supply Shortages
Many Americans come face to face with these shortages when they seek a new primary care provider or request an appointment and are quoted a multi-week wait time or told the doctor is not accepting new patients. These realities force patients to ignore their most basic healthcare needs or delay care. Nationally, there is a significant shortfall in healthcare providers, exacerbating the challenges of ensuring timely healthcare services for patients.
In 2022, McKinsey’s healthcare labor market report found that “the United States may confront a shortage of 200,000 to 450,000 registered nurses and 50,000 to 80,000 physicians by 2025 as demand for care rises and supply lags.13 Reversing this trend will require health systems to take a multi-pronged approach to recruiting, retaining, and retooling their workforces, and to meet the needs of their frontline workers effectively and compassionately.” The shortages across healthcare can and will significantly affect patients and providers alike.
McKinsey is not alone in warning about a looming doctor shortage. According to a 2024 report from the Association of American Medical Colleges (AAMC), the total physician shortage is projected to be between 13,500 and 86,000 by 2036.14 Those projections are below AAMC’s 2022 report, which projected up to 120,000 physicians short by 2030 but should still prompt concern by patients and policymakers.15
The wide range in the AAMC’s shortage projections reflects different assumptions about the demand for care and the production of new physicians by medical schools. The lowest projection assumes Congress will drastically increase federal funding for graduate medical education (GME), better known as residencies. Such funding would create thousands more residency slots, but this expensive federal policy change has not garnered significant support in Congress to date. The highest shortage projection assumes a more static supply of providers, with little increase in medical school graduation that may be unable to keep up with the departures of aging physicians leaving practice at retirement.
However, shortage calculations do not merely rely on the supply of doctors. Instead, the demand for healthcare services is also a key variable. Notably, the AAMC baseline for “adequate supply” of physicians merely identifies the total number of providers needed to provide a minimal level of care under current population and demographic changes. That same report finds that the projected shortage would be even higher, in the neighborhood of over 200,000 physicians, if the level of healthcare demand were equal to a more idealized level, equivalent to the level of care demanded by those in suburban portions of America.16
Importantly, any model that merely looks at the total number of providers per capita fails to account for the ever-increasing healthcare needs of the aging and less healthy population. Shortages get worse given the significantly older population’s higher healthcare use, higher rates of physician specialization, and reduction in hours spent caring for patients per doctor. Shortage projections are based on all of these factors, which, unfortunately, are all trending toward larger and larger shortages both now and for years into the future.
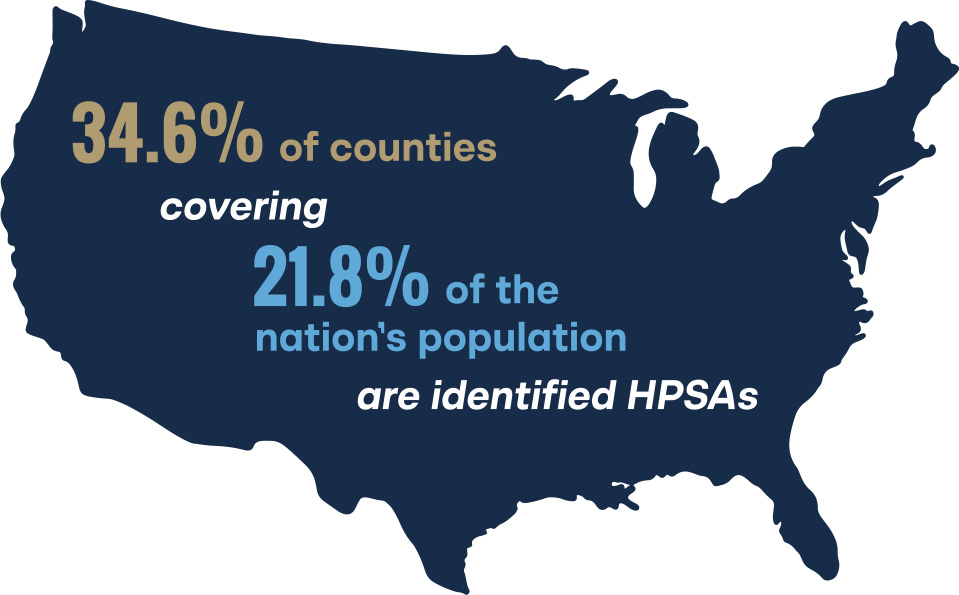
Regardless of which assumptions best predict future shortages, the ultimate conclusion remains the same: American patients will have more difficulty finding a doctor in the years ahead. The U.S. Department of Health and Human Services’ Health Resources and Services Administration estimates that some 1,088 counties in the United States—a full 34.6 percent of counties covering 21.8 percent of the nation’s population—are federally identified Health Professional Shortage Areas (HPSA).17 An HPSA is defined as a county or local community with a ratio of primary care providers to population of one to 3,500 or less.18 This number varies depending on the needs of the community, calculations that rely on more local demographic data. Some states, like Louisiana, New Mexico, and Maine, have fewer than five counties that are not HPSAs.19,20,21
A recent study from the Paragon Health Institute argues that the method to identify federal HPSAs is outdated and may not reflect the growing ability of other healthcare providers to meet healthcare needs.22 Nurse Practitioners and Physician Assistants play a vital role in care delivery and these professions have added some 600,000 providers since 1980. However, even with these additional providers, many care gaps remain that will only worsen in the years ahead. Absent these providers, the shortages would be even worse. While some shortage measurements may rely on outdated methodology, the trend lines of both anecdotal and analytical analyses show that America’s physician shortage is on the rise, and patients cannot afford to disregard shortage designations merely due to criticism of their methodologies.
Projections of primary care shortages are less variable across assumptions and over the AAMC study’s bi-annual iterations, with a range of 20,200 to 40,400 physicians short.23 The primary care shortage is even more acute in individual states, where specific regions may experience a more severe lack of primary care physicians, hindering the delivery of essential medical services.24
In addition to the primary care shortage, the patient care today demands more specialists than ever before. The AAMC predicts a combined deficit from surgical specialties, internal medicine subspecialties, emergency, and peri-operative specialties reaching up to 44,900 physicians by 2036.25 This deficit in specialized medical fields poses a formidable challenge to meeting the diverse healthcare needs of the aging population.
The Health Resources and Services Administration also projects severe shortages in multiple additional subspecialties over the next decade, with non-metro areas being the worst off.26 At the state level, particularly in rural areas, this scarcity is even more palpable. Across all specialties, non-metro areas are projected only to have 48 percent of the number of physicians necessary to care for their population, compromising the ability to address complex medical conditions effectively.
Finally, most studies of physician supply fail to account for non-patient care work some doctors now perform. Some doctors work for insurance companies, pharmaceutical companies, and other fields but rarely, if ever, dedicate their time to patient treatment. Some doctors nearing retirement or seeking to balance work, family, or other obligations work less than full-time. Still, other doctors have quit practicing altogether but maintain their licenses. These realities mean that most estimates of the physician shortage that rely solely on the total number of licensed physicians rather than a more nuanced calculation using hours dedicated to patient care will underestimate the actual shortages.
State-level Shortages
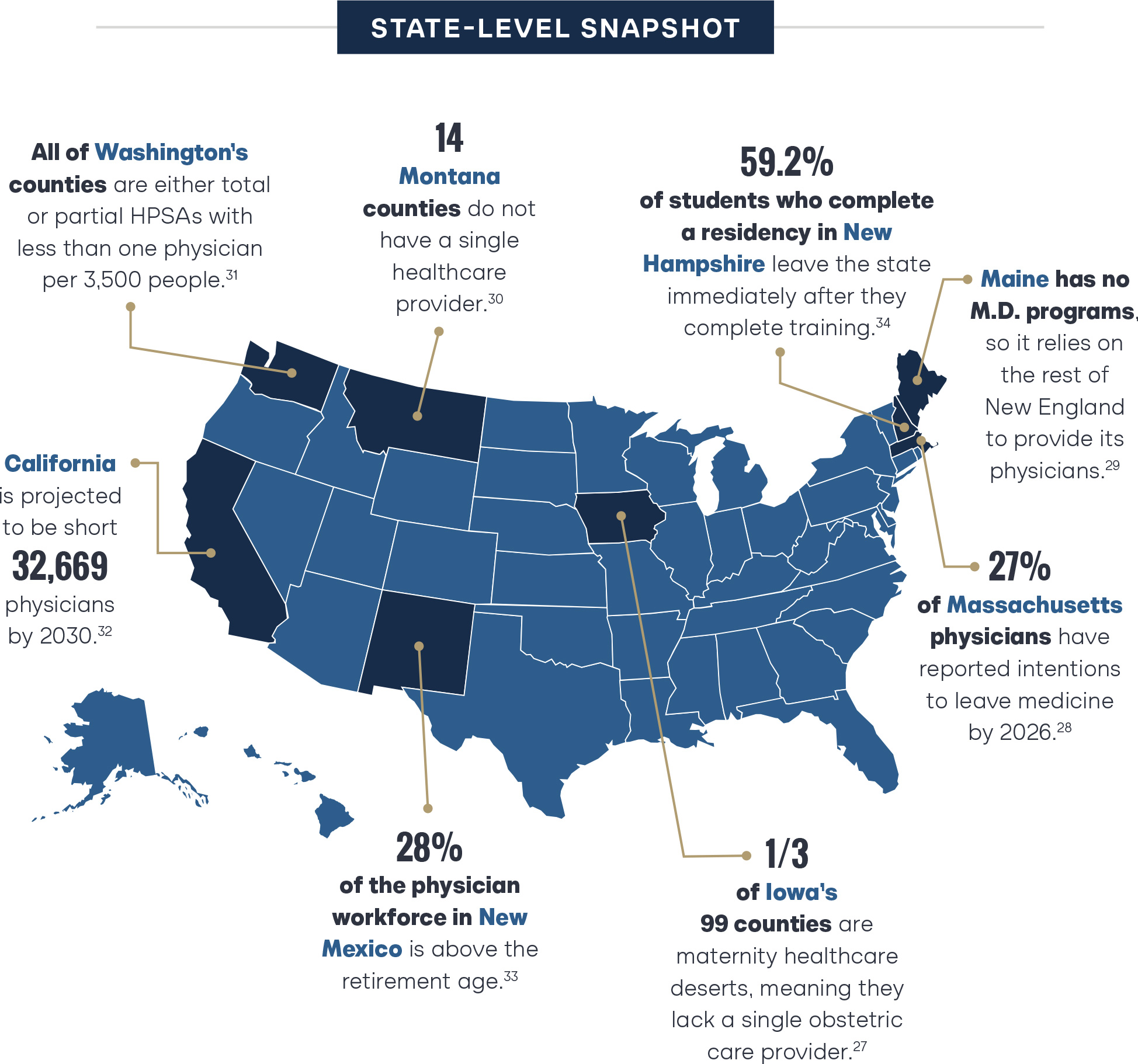
The national data on healthcare provider shortages are troubling. However, many states face even more significant shortages relative to their populations. Further, even some states with relatively small shortages have doctor practices concentrated in particular regions of the state, with more rural communities facing more considerable shortages. Luckily for the citizens of those states, physician licensing is a state activity, and their state elected officials have the power to address these shortages.
Below is a sample of some critical provider shortage data from across the states.
Consequences of Physician Shortages
The physician shortage has far-reaching consequences. Delayed patient care is one of the most immediate impacts. As the demand for medical services outpaces the available supply of physicians, individuals may experience prolonged waiting times for appointments and treatments.35 According to the longest-running physician wait-time survey, wait times for OB/GYN appointments are up 17 percent from 26.4 days to 31.4 days since 2017.36 New patient primary care appointment wait times are up to an average of 26 days.37 Growing wait times have the potential to compromise health outcomes. Kicking the can down the road by delaying care is not an adequate solution to a lack of service, especially if the foot doing the kicking is being affected by diabetic neuropathy.38

Without adequate local or telehealth optionsi, many patients must travel long distances to access essential healthcare services.39 In areas where the shortage is acute, individuals may be compelled to journey considerable distances (in some cases 70 miles or more), imposing a substantial burden in terms of time and money, especially on those who are already grappling with health challenges.40 This geographic barrier to healthcare not only strains patients but also contributes to disparities in access, disproportionately affecting residents in rural or underserved regions.
iThe Cicero Institute has long advocated for broadening access to telemedicine services and publishes an annualreport on the progress states are making to improve telehealth access.
Delays due to geographic access and overall physician availability amplify the risk of medical complications. Having fewer providers also increases the likelihood of delayed diagnosis and intervention, exposing patients to elevated medical risks. This heightened vulnerability can lead to more severe health outcomes, as timely medical attention is critical to prevent complications and ensure effective treatment.41
The physician shortage also has an economic impact. Increased demand for medical services coupled with falling relative physician supply contributes to rising healthcare costs. On top of that, it is very costly to delay treating acute medical issues that could be easily addressed by a primary care provider, especially when the patient winds up in the emergency room or develops chronic ailments.42 Without the consistent intervention of preventive medicine provided by a primary care doctor, conditions that would have been treatable end up costing an average of $2,032 in a hospital ER.43 The strain on the system increases financial burdens on both individuals and the healthcare infrastructure, potentially limiting access to care for economically disadvantaged populations.
Patients would be healthier if they had more visits to the doctor. Unfortunately, the doctor shortage puts everyone in a catch-22. Increasing the use of already scarce healthcare provider resources would further drive up the physician shortage. Not accounting for the initial increase in burnout that would occur, moderate estimates suggest that if healthcare use increases in rural areas to approach a “suburban” use level, the shortage will approach a whopping 200,000 physicians across all fields.44
Furthermore, the shortage places a substantial burden on existing healthcare practitioners who find themselves stretched thin. Overworked physicians and other healthcare professionals face burnout, compromising the quality of care they can provide. The increased burden on the current workforce affects their well-being and enforces a cycle of exhaustion, further exacerbating the challenges associated with the physician shortage. In 2023 alone, 29 percent of medical group leaders reported physicians retiring early due to burnout.45
Causes of Physician Shortage
Population Growth and Longer Life Expectancy
The U.S. population is getting larger and older. Population age and size have been trending upward for decades and are expected to increase even faster in the years ahead. These trends will continue as the physician workforce simultaneously declines. Total U.S. population is projected to increase by 8.4 percent by 2036, but that is not the most startling statistic.46 The population aged 65 and older accounts for a disproportionate share of population growth over that same period. That cohort is expected to see a 34.1 percent increase, while the population over 75 will likely see a 54.7 percent increase.47 Older age cohorts have significantly higher demand and need for healthcare services which will lead either to increased costs or further delays in care.48 The need for specialty care in this population is likewise higher, which amplifies the gaps in available care amongst different physician specialties.
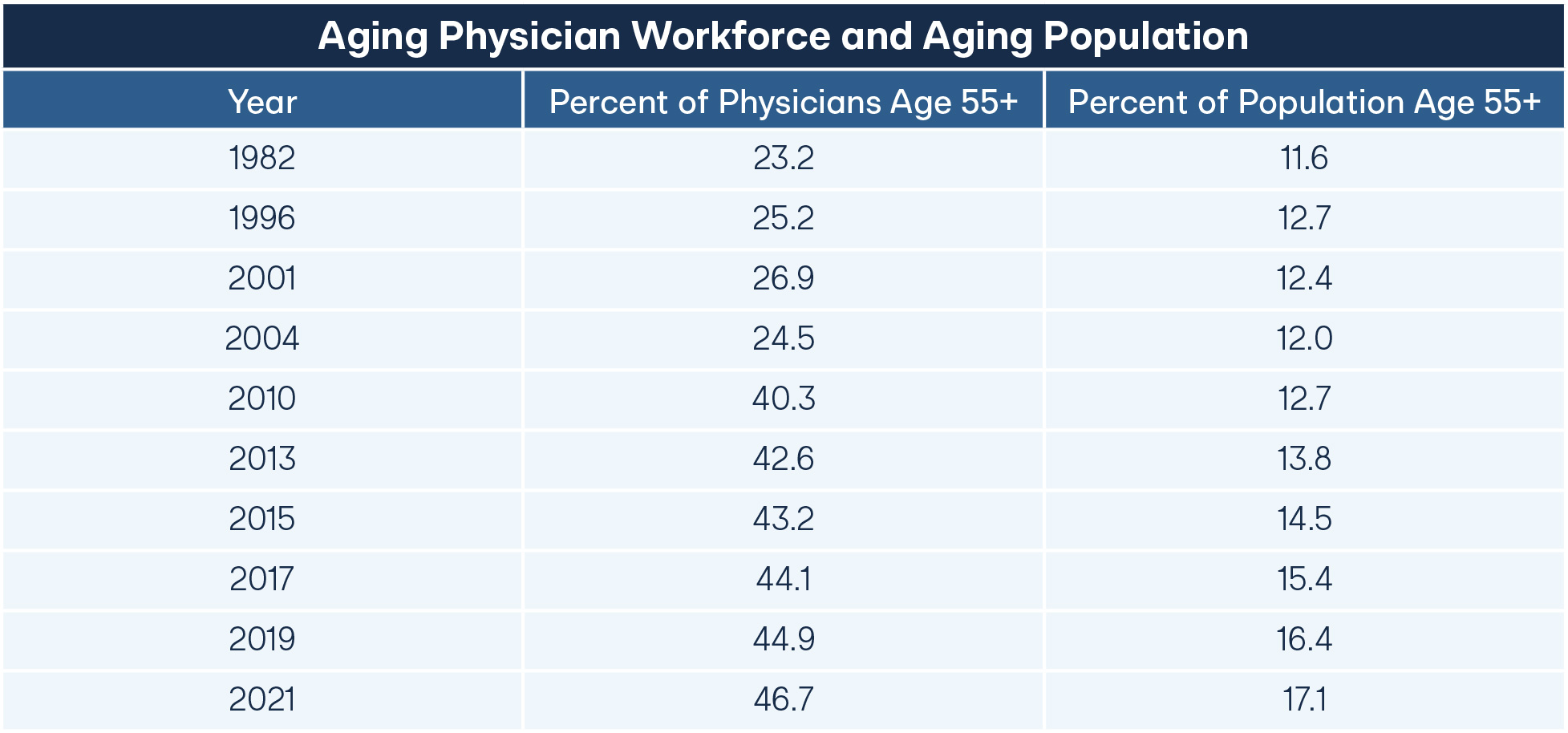
Physician Burnout and Retirement
The pandemic not only underscored existing disparities in health and healthcare access but also took a toll on the physical and emotional well-being of physicians and healthcare workers. According to the American Medical Association (AMA), two in three doctors reported burnout during the pandemic, causing many physicians to explore ways to reduce their hours worked or change careers entirely.49 The most recent survey data from the AAMC indicates that between 2019 and 2022, a plurality of physicians have changed course and plan to retire earlier than previously expected.50 Since nearly half of all physicians practicing in the U.S. are 55 or older, doctors retiring earlier than previously expected could be catastrophic for physician supply in the short term.51 As discussed above, if physicians retire but maintain their licenses they may still be counted as part of the physician workforce even though they do little to address physician demand.
Changes in retirement age can play a significant role in increasing or decreasing the physician shortage. In 2015, the Annals of Family Medicine published a study that projected the 2035 primary care physician shortage to be 33,283, assuming doctors retired at age 66. To show that retirement age matters, they re-ran their model for a slightly earlier and slightly later retirement age. The authors conclude that “If primary care physicians retire at age 64 years, the shortage increases to 38,622, whereas delaying retirement until age 68 years contracts the shortage to 26,835.”52 As more doctors cite burnout and a desire to exit the practice post-pandemic, the need for new doctors to fill the ranks of those retiring will only grow.
Alternative Career Pathways for Doctors Attract Talent
In recent years, medical school graduates are choosing alternative career pathways. Reports find that roughly 25 percent of medical students and physicians are actively considering leaving the practice of medicine for non-clinical careers.53 Despite still fierce competition for seats in medical school, many talented medical graduates are attracted to alternative careers that offer significantly better lifestyles compared to grueling residency and fellowship training and a career with alarming burnout rates.54 Additionally, with the average American medical graduate holding roughly $250,000 in student loans, many talented students and physicians may consider the real and opportunity cost of an extended series of training steps too steep compared to the value proposition of alternative careers that offer immediate compensation at higher levels. Over a fifth of all physicians in the U.S. are employed at least part-time as consultants for corporations because those roles allow doctors to earn more than they would spending that time in a traditional clinical setting.55
Limited Training Slots (Medical Schools and Residency Slots)
As current doctors retire and the population grows, newly trained doctors are needed to fill their seats. The main talent pipeline for medical training continues to be medical school and residency. However, even as medical schools have been adding seats and producing more graduates than ever before, graduate residency slots are still precious and limited.56 And since newly minted medical school graduates can only practice after they complete a residency, the number of residency slots may be more impactful on the shortage than the number of seats in medical schools.
The majority of residency program funding comes through Medicare and Medicaid, with a small number of state-and privately-funded options.57 For example, teaching hospitals will often train additional residents through state funds and other private funding sources to try and meet the needs of their patient populations. The number of federally-funded residency slots (graduate medical training) was capped in 1997.58 This cap means that despite significant population growth, the number of new fully trained doctors available to patients has not grown significantly for nearly three decades. Specifically, the total number of residency positions has risen from 98,143 to 107,708 from 1997 to 2023, a reduction in the number of residency positions per capita, and much of this small increase is due to state or private funding rather than federal increases.59–60
Further, the capped funding locked residency geography into place. Despite regional shifts in population, the residency slots remain allocated based on the needs in 1997. As such, residency slot allocation no longer reflects the population demographics or demand for physicians consistently across the nation. Arizona, for example, is now the 14th most populous state in the United States but still ranks 37th in total residency slots. According to the University of Arizona, “Arizona would need to increase the resident physician workforce by about 1,000 positions to attain a rank of 15th by ratio of resident physicians per 100,000 population.”61 Some members of Congress recognize these challenges and have tried to make small, targeted efforts to improve training program capacity in areas of particular need.62 The results of these efforts have been mixed at best, with most newly created slots still not going to rural residency training programs.63–64
The limited number of residency slots means thousands of medical graduates fail to secure a residency training program in their preferred specialty each year. Most recently, in the 2024 Match, almost 9,000 certified doctors were unable to secure a residency position and enter further training.65 There is no shortage of qualified talent wanting to continue their training to become physicians or surgeons. Currently, fully licensed international physicians are vying for the same limited spots that medical school graduates compete for, often with high success rates as they have more experience and are able to attain higher scores on the United States Medical Licensing Examination (USMLE). Rather than limiting physicians by keeping these two very different sets of candidates in the same pool, developing an alternative route for IMGs could result in more physician availability across the country.
Physician Supply Pathways
The path to become a licensed doctor seeing patients in the U.S. is long and varies based on where a physician has trained. The average American-trained doctor will complete an undergraduate degree, medical school degree (MD or DO), medical residency, and possibly a subspecialty fellowship, taking at least 11 and sometimes more than 15 years before receiving their license and being able to independently care for patients in their desired specialty.66
Residency is post-graduate practical training in a particular medical specialty. Doctors apply for residency during their final year of medical school and “match” to a residency in the spring of their final year. There are currently 160 different residency specialties to choose from, ranging from abdominal imaging radiology to vascular surgery.67 The length of residency programs varies from three to seven years, depending on specialty.68 Pediatrics residency is a three-year program, while neurosurgery is a seven-year program.
There are currently 153,883 doctors in residency programs in the United States. Two-thirds of them are in the 10 most popular specialties:
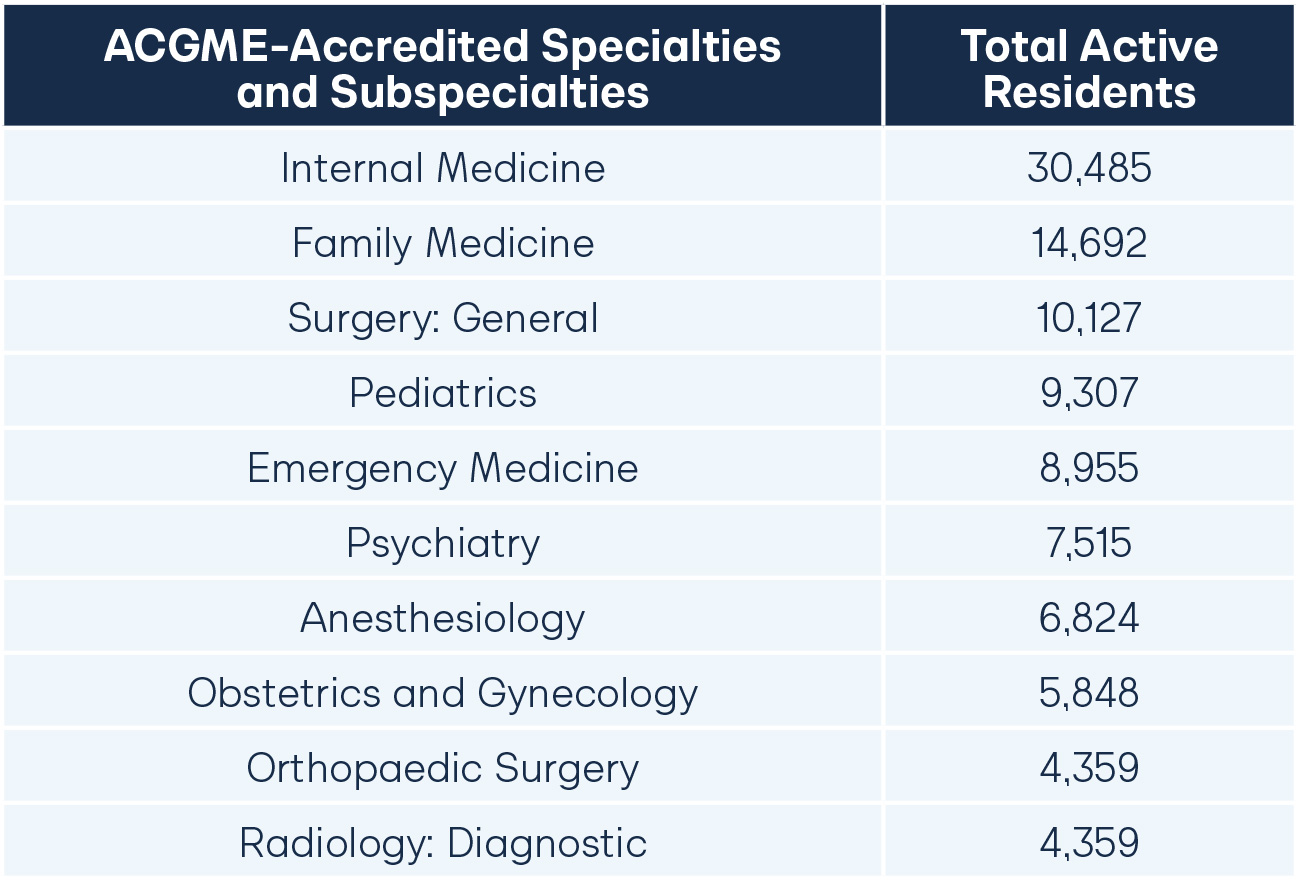
As the following charts confirm, the following five specialties make the top 10 for both IMGs and U.S. medical school graduates: internal medicine, family medicine, pediatrics, general surgery, and psychology. Emergency medicine residencies, on the other hand, are composed almost entirely of graduates of U.S.-based medical schools (8327 of 8955). Among the 10 most popular specialties, graduates of U.S.-based medical schools make up more than 90 percent of all residents in emergency medicine, anesthesiology, obstetrics and gynecology, and orthopedic surgery (where they make up 99 percent).
International Medical School Specialization:
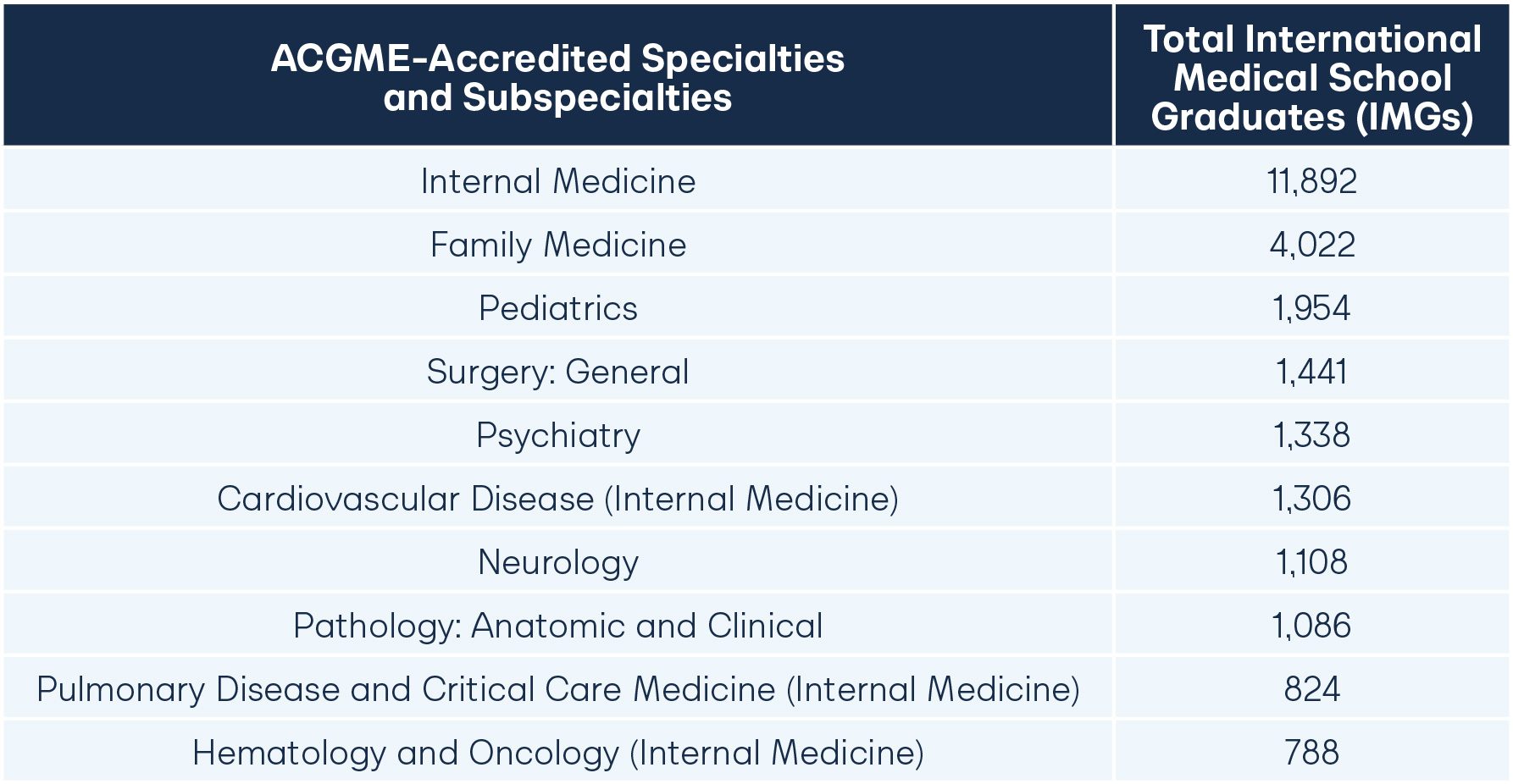
U.S. Medical School Specialization:

Doctors who train abroad and want to practice in the United States must compete with American graduates for the limited residency positions to work as doctors in the U.S. Even doctors trained outside the United States who have already completed postgraduate specialty training must complete a U.S.-or Canada-based residency. This is because the state licensing rules have refused to recognize postgraduate training in other countries. This dynamic is changing rapidly in 2024, with many states coming to realize that experienced foreign doctors can help alleviate their physician supply issues.69 A handful of states are enacting new laws that integrate experienced foreign doctors into the workforce in safe and measured ways that do not use up the limited residency positions available or impose redundant training requirements on the doctors.70
Ways to Address Physician Shortages
It is abundantly clear that there is a growing physician shortage across geographies and specialties in the U.S. Demand will continue to increase, leaving state legislators to identify solutions to the shortage. This section identifies some legislative actions that can help meet this demand.
Open the Door to Telehealth
Telehealth and increasing telehealth access are essential ways to address some of the consequences of the physician shortage right now. While telehealth is not a catch-all replacement for in-person visits, it can go a long way to free up physicians and healthcare facilities to handle higher volumes of patients. Telemedicine can mitigate geographic and travel constraints for those with access to technology, and it lets patients consult with specialists hours away without taking too much time away from work and other responsibilities.71 Current unnecessary barriers to telehealth exacerbate the shortage in many rural areas. Several states are developing legislation to dismantle these barriers, such as allowing multimodal telemedicine, access across state lines, and increasing provider options.72
Expand the Scope of Practice To Allow More Physician Assistants, Nurse Practitioners, and Pharmacists To Perform “Doctor-Like” Work
Physician Assistants, Nurse Practitioners, and Pharmacists are provide healthcare to millions of patients across the country and help meet the high demand for healthcare, often with improved quality metrics and health outcomes, particularly in underserved communities.73 By expanding scope of practice for these allied health professionals, physicians would be able to concentrate on cases that are matched to their specialist training. While many laws are currently being enacted to expand the scope of practice for allied professionals, many physician groups advocate for supervisory limitations to avoid compromising the quality of care.74 This debate is not unique to the U.S.; the blurring of the lines between seeing physicians and allied professionals has stirred intense debate in the UK following fatal mistakes in patient care from poor supervision and the independent practice of Physician Associates.75,76,77
Increase the Number of Doctors Being Trained by Adding Seats in Medical Schools and Residency Programs
Another approach is to expand the number of medical school and residency positions. More seats in these programs would increase the pipeline of physicians in the U.S. Some states have pursued this approach by using state budget resources to train more doctors in the state. The 2023 Arizona state budget included funding to increase residency program capacity, with a particular focus on community medicine and rural healthcare.78 The ability of programs such as these to retain doctors in underserved communities is yet to be monitored. The most recent data indicate that Arizona retains roughly half of the students who complete a residency program in the state.79 If that statistic holds true, the budget would need to fund two residency slots for every one doctor who would serve Arizona citizens in the long term.
Arizona is not alone in this trend of doctors training in one state but practicing in another. The American Association of Medical Colleges reports that more than 40 percent of students choose to change states after they complete their residency training: “Overall, 57.1 percent of the individuals who completed residency training from 2013 through 2022 are practicing in the state of residency training. Retention rates range from 38.5 percent in the District of Columbia to 77.5 percent in California.”80
At the federal level, there is some recent movement in the form of the 2023 Resident Physician Shortage Reduction Act, which proposes to add 14,000 Medicare-funded residency positions, again focusing on underserved areas.81 At the time of publication, this bill is still awaiting a hearing in the House Subcommittee on Health and appears unlikely to become law in this Congress. Ultimately, these efforts will rely on significant additional funding, bureaucracy, and strategic planning to impact the physician shortage.
While increasing medical school admissions and residency slots can help reduce physician shortages in the long run, it still often falls short of addressing the specific challenges faced by rural states. The ineffectiveness stems from various factors, including the maldistribution of healthcare resources, the lifestyle preferences of medical graduates, and the complex nature of rural healthcare practice.82 Merely expanding educational opportunities may be insufficient to attract and retain physicians in rural areas, as these regions often grapple with issues such as limited infrastructure, professional isolation, and fewer opportunities for spousal employment.83 To fully address rural state-specific shortages, a comprehensive approach may be needed, encompassing targeted incentives, community engagement, and tailored support systems that address the unique needs and challenges of rural healthcare delivery.
Provide a Practice Pathway for Medical School Graduates Who Do Not “Match” to a Residency Program
Each year, the vast majority of medical school graduates “match” into a residency program. However, the 6.5 percent of MD graduates and 7.7 percent of DO graduates who did not match in 2024 still amount to 1911 graduates of U.S.-based medical schools.84 While these graduates can certainly apply to match again in subsequent years, their placement rates are significantly lower, meaning a large number of these graduates may never obtain a residency match. And, absent an eventual match, these graduates are unable to take on any significant role as a healthcare provider.
Some states have created programs to give these medical school graduates an opportunity to work in medicine. These programs address the plight of partially-trained but not license-eligible medical school graduates and leverage the knowledge and skills of these additional healthcare workers to treat patients.
States like Missouri, Idaho, Arkansas, Arizona, Utah, and Louisiana have created the Assistant Physicians category.85 Assistant Physicians are medical graduates who have completed Steps 1 and 2 of the United States Medical Licensing Exam but have yet to enter into a residency program. They work under the supervision of an attending physician but are employed in a clinical setting as they prepare for the next cycle of the residency match. This type of program significantly improved primary care provision in Missouri, with almost 300 Assistant Physicians being employed in the state in 2023.86 While this arrangement can plug some primary care gaps, it is limited in scope and scale because Assistant Physicians must practice under a fully licensed physician and, in some cases, can only renew their limited licenses for a handful of years. At this time, no assistant physician could become a fully licensed physician unless she or he completed a residency program before she or he then applied to obtain a license to practice medicine independently.
Washington’s Assistant Physician program is open to International Medical Graduates (IMGs).87 This program gives IMG physicians the opportunity to integrate into the American health system and develop cultural competencies while also contributing to the provision of care in areas of need. However, this might not be the best deployment of IMGs, particularly for those who have completed specialty training abroad, since it focuses on primary care delivery, not specialty care.
Responsibly Recognize Foreign Medical Licenses Without Requiring Repetitive Postgraduate Training
The U.S. is amongst the most desirable countries to work for physicians trained anywhere in the world. Currently comprising roughly a quarter of the U.S. physician workforce, IMGs are drawn to the earning potential, academic rigor, and physical and electronic healthcare infrastructure that accompany practicing in the U.S.88 This desire has become a critical foundation for healthcare services in underserved and rural areas where foreign-trained physicians make up more than a third of all doctors.89 Florida and California currently have the highest concentrations of IMGs, thus ranking in the top half of states in total physician supply.90
IMGs traditionally attend medical school outside the United States and then apply to U.S.-based residency programs for specialty training. These doctors often have graduate degrees or additional training before they arrive in the United States for a residency program. Most of these physicians receive training in India, the Caribbean, Pakistan, the Philippines, and Mexico.91 New Jersey and New York have the highest percentage of IMGs, nearing 40 percent of their entire physician workforce.92 On the other hand, Utah, Montana, and Idaho each have less than 10 percent IMGs in their physician workforce and fewer primary care physicians per 100,000 patients than the national average.93
One promising option to quickly expand the U.S. physician workforce is to allow internationally-licensed physicians to practice medicine in the United States. There are already a handful of doctors licensed abroad who practice in the United States and never completed a U.S.-based residency. Still, barring special circumstances, most states will not license a doctor unless the doctor completes residency training in the United States or Canada. State medical boards and legislatures can find creative ways to reduce these barriers, and doing so could help alleviate the physician shortage. One significant advantage of licensing internationally-trained and already practicing physicians is that they can start to work in the United States immediately without completing any additional training. Adding a new residency slot, by comparison, will take at least three years to produce a new practicing doctor. And adding a new medical school seat and residency slot will take at least seven. But if state laws can recognize equivalent foreign training, an internationally-licensed doctor who is a U.S. citizen or arrives as a refugee can begin practicing immediately upon licensure.
International Physician Licensing
Doctors jump through dozens of hoops to obtain a license to practice. State licensing laws vary, but generally, every state requires a doctor to complete an undergraduate degree, graduate from an accredited or otherwise recognized medical school somewhere in the world, complete graduate medical education (GME) in the United States or Canada, pass all three steps of the USMLE or MLE, and complete an application process with the state medical board that generally includes a background check and application fees.ii Doctors who are not U.S. citizens, or even citizens who complete medical school outside the United States or Canada must often complete additional steps in the process and many states require those doctors to complete additional years of residency training before they can apply for a license.94
iiIt is important to note that licensing in a state is a separate process from specialty board certification.
Tex. Occupations Code § 155.001-155.151 (2023), https://statutes.capitol.texas.gov/Docs/OC/htm/OC.155.htm.
Colo. Rev. Stat. § 12-240-110 (2023), https://leg.colorado.gov/sites/default/files/images/olls/crs2023-title-12.pdf.
Okla. Stat. tit. 59 O.S., § 480-518 (2023), http://www.oklegislature.gov/osStatuesTitle.aspx.
Ariz. Rev. Stat. § 32-1422 (2023), https://www.azleg.gov/viewdocument/?docName=https://www.azleg.gov/ars/32/01422.htm.
N.J.A.C. § 13:35-3 (2024), https://www.law.cornell.edu/regulations/new-jersey/title-13/chapter-35/subchapter-3.
As discussed above, thousands of American doctors graduated from medical schools outside the United States. In some countries, that training is expedited vis-a-vis the eight-year process most students complete in the United States (undergraduate followed by four years of medical school). For example, Indian medical schools combine undergraduate and medical school education and take five and a half years to complete.95 Brazil and many European countries have six-year programs that similarly begin immediately after secondary school.96
Until recently, no matter where you went to school, how many years you had to go, or whether you had any unique additional training or experience, the baseline requirement to practice medicine in the United States always included a U.S.-or Canada-based residency program for at least one year. Any exception to this rule required either a special employer (e.g., a university medical school) or a waiver from a medical board. [SEE FIGURE A.]
Yet, as physician shortages grow, some states have begun to look for innovative solutions. One category of potential talent was doctors who had practiced medicine in other countries for a number of years but were interested in moving to the United States to practice. However, a U.S.-based residency requirement poses the most significant barrier for those doctors. As such, some states have begun questioning the need for residency for well-trained, experienced physicians. If coupled with the right parameters, such a program can increase the quantity of physicians in a state without risking patient safety.
The Current Process
The path to a medical license in the U.S. is not trivial for doctors trained abroad. The primary gatekeeper is the Educational Commission of Foreign Medical Graduates (ECFMG), a body that ensures that a prospective doctor from abroad has completed an accredited medical school curriculum and achieved a satisfactory score on the USMLE exam. Once ECFMG certified, a doctor from abroad can enter the competitive residency match pool and interview for a spot in a postgraduate training program.
Each year, roughly 13,000 ECFMG-certified International Medical Graduates (IMGs) apply for a residency.97 In the last two years, 8,388 and 7,670 IMGs have successfully matched to residency programs, respectively. Following the assignment of an IMG to a residency program, the doctor needs to apply for a visa (unless that doctor is already a U.S. citizen or green card holder). IMGs choose between different types of visas.98 The process of organizing visas has always been complicated and time-consuming, which adds to the complexity of recruiting international physicians for residency programs and practice in the U.S. Added to this complexity, one of the most common residency visas for IMGs is the J-1 visa, which requires a physician to return to their home country for two years following their medical residency. This means the U.S. patient population would not benefit from the expensive training of freshly certified physicians for two years.
The Conrad 30 Visa Waiver Program was introduced in 1994 to remove this requirement to allow some physicians trained in a residency to continue their practice as attending physicians without returning to their home country. The program has been limited in scale but expanded in 2002. The National Bureau of Economic Research has investigated the effects of this program until 2020 for evidence of “crowding out” the opportunities for U.S.-born physicians, one of the key concerns from physician groups against the expansion.99 Their analysis found that the waiver increases the supply of physicians in Health Professional Shortage Areas (HPSAs) without affecting the number of U.S.-born physicians in the states where the cap was expanded. Furthermore, recent 2024 polling also suggests that Americans broadly support simplifying the process for foreign doctors to stay in the U.S., where they can contribute to the care of rural and underserved communities.100
But regardless of visa type, these licensing pathways are designed for brand-new doctors, not those with years of experience. Doctors who choose to complete residency training outside the United States or Canada and subsequently practice outside the United States look different, but with few exceptions, must follow the same path. Because this path is burdensome, most doctors outside the United States simply choose to remain in their current country or, if they come to America, decide to set aside their medical training for alternative careers.
There are, however, a handful of programs designed to allow internationally-licensed physicians to care for American patients. First, many states permit internationally-licensed doctors to practice so long as they are on the faculty at a university. Washington, Texas, and New York all have statutes that allow such licensure.101 Other states have programs that allow doctors who do not meet all of the state’s requirements to practice at a specific facility.102 And California has allowed 30 Mexican doctors to work in community health centers on nonrenewable three-year licenses under a program passed more than 20 years ago under AB 1045.103 While most of these programs do not allow a doctor to earn a full and unrestricted license for practice, they do demonstrate that U.S.-based residency programs are not absolutely essential for a doctor to meet state medical boards’ or state legislatures’ standards of competency to practice medicine.
Pathways to Full Medical License
States should create pathways for internationally trained physicians to provide care in the U.S. on a full and unrestricted basis without repeating residency in the United States. Ideally, states take a sponsorship approach where licensed doctors and healthcare providers in the state hire internationally-licensed physicians for a probationary period and the medical board ultimately grants successful doctors a full license. States can and likely will still require these doctors to prove their competency and fulfill all other licensing requirements except a residency. Such an approach ensures these “new” doctors are thoroughly trained, mentored by experienced local physicians, and able to progress to full independent practice.
Importantly, the pathway should culminate in the opportunity for the internationally-licensed physician to become fully licensed in the state.
The pathway to full practice for a foreign-licensed doctor should be just as rigorous as the pathway to practice for a doctor trained in the United States. Doctors licensed abroad should still be required to demonstrate, to the satisfaction of the state medical board, that they have the skills, training, and experience to practice medicine in the state and, once they demonstrate it, should remain subject to the jurisdiction of the medical board and follow the same rules as every other doctor in the state. The only requirement that should change vis-a-vis American-trained doctors is the elimination of redundant residency training.

This section explains these features and their justifications:
Sponsorship
Sponsorship provides a few key benefits for a licensing program. First, it ensures the doctor has employment and mentorship as she transitions to practice in a new country. Second, it provides a second set of scrutinizing eyes to ensure the doctor has a sufficient level of skill, training, and experience to practice medicine in the state. Third, it allows the new doctor to focus on patient care rather than learning insurance billing and practice administration.
Each doctor must have an offer of employment from an in-state licensed healthcare provider that enters into a sponsorship agreement with the doctor to take on liability and provide cultural competency training. Ideally, the sponsorship agreement would be with an individual doctor and not just from a facility or entity that employs doctors.
Approved Medical School
The Education Commission on Foreign Medical Graduates (ECFMG) already collects transcripts and proof of graduation for doctors trained in medical schools outside the United States to share with residency programs and state medical boards. States can utilize this same process for doctors licensed abroad who wish to prove their credentials to a state medical board via this alternative pathway. ECFMG regularly monitors and evaluates medical schools around the globe, and some are not qualified for ECFMG approval.
Further, it is essential that any legislation not exclude doctors who complete medical school in the United States but then attend residency and obtain a license outside the United States. Because not every student matches into a residency during medical school, some doctors licensed outside the United States attended medical school in the United States, completed residency abroad, and then became licensed in a foreign country as well. Other doctors may have returned home, followed a spouse or family member, or faced other hardships that required them to leave the United States. However, the choice to attend a U.S.-based medical school and then obtain a license outside the country should not be a barrier to pursuing the international physician licensing pathway.
Passing USMLE Scores
Doctors who attend medical school in the United States or outside the country take the USMLE exams to prove their medical knowledge.i Passing scores on all three steps of the USMLE exams are prerequisites to traditional medical licenses in every state. One option lawmakers have when considering licensing practicing doctors from abroad is whether Step 3 should be required before a provisional license is granted or only before a full license is issued. On the one hand, Step 3 is the most hands-on and practical of the assessments and can provide a valuable screening mechanism to ensure not only the basic knowledge of the doctor but also their ability to care for patients. On the other hand, because Step 3 is so practical, it may be more reasonable to give the doctor a few years of provisional license experience in the United States first before such a skills assessment.
An IMG who wants to apply for a residency in the United States already must complete medical school at an approved school and pass the USMLE exams. These existing ECFMG standards must be met before an IMG can obtain an ECFMG “certification” and apply for residencies in the United States. For an internationally-licensed doctor with experience, the ECFMG certification process is still a valuable way to confirm the doctor has proven his or her training and demonstrated the knowledge required for a license in the United States.
Completion of a residency or post-medical school training program
Medical school provides an excellent foundation in the knowledge a doctor needs to practice medicine. Still, post-medical school hands-on training is where most young medical school graduates actually learn to practice medicine. This is true both in the United States and in most other countries. As such, it is essential that any doctor who seeks to practice medicine in the United States complete postgraduate training in their specialty. In some countries, a formal “residency” or “fellowship” is not required. In those cases, treating the first five years of practice as an equivalent to residency is recommended. Requiring residency training (albeit outside the United States or Canada) ensures doctors who move their licenses to the United States have the specialized training that completes their formal education.
Some might argue that residency training in the United States is so unique that foreign doctors are not actually “repeating” their training when they enroll in a residency training program. The Cicero research team investigated residency programs in the United Kingdom and India and identified overlapping training requirements with residency programs in the United States.104 This investigation of residency variation finds that residency programs around the world cover many of the same topics. Furthermore, this research finds a wide variation in the material U.S.-based residency training programs cover. For example, a rural emergency department residency will have a very different practice profile from an urban emergency department residency. Despite the significant differences, no state requires a doctor with a residency in a rural area to repeat training to practice in the urban areas, or vice-versa. Given the similarities between most international programs and most U.S.-or Canada-based residency programs, it seems much more fitting to simply require an IMG to work with his or her employer to obtain any additional training to fill gaps, just as the urban-trained doctor might do when she moves to a rural area.
Competencies
In family medicine, the ACGME family medicine residency requirements make 63 statements outlining competencies related to patient care, procedural skills, professionalism, medical knowledge, practice-based learning, interpersonal and communication skills, and systems-based practice.105 The UK General Practitioner Training Guidelines highlight 60 of the same competencies within their own training requirements documentation.106 Similarly, India’s MD in Family Medicine requirements refer to 59 of the same competencies outlined by the ACGME.107

Skills
When comparing procedural skills training requirements for pediatric residents in India against the U.S., residency training in India requires competency in 14 of the 15 procedural skills set out by the ACGME in the U.S. At the same time, the UK highlights 10 out of 15.108–109 Several procedures are explicitly required in the Indian and UK programs but excluded from the American requirements, such as performing a bone marrow biopsy and suprapubic aspiration.

License To Practice in a Foreign Country
Not only should a doctor be a medical school graduate and complete post-graduate residency training, but that doctor also should have a license in good standing without pending discipline or investigations in their country of practice. This assures that the doctor’s practice abroad is aligned with local rules and regulations and does not endanger patients.
Some doctors, especially refugees, may have significant difficulty proving their license remains in “good standing” in their former country. For this reason, states may want to grant the medical board some discretion to waive this requirement in extenuating circumstances. Similarly, some doctors may not apply for a license while still in their licensing country, which could mean that a license may expire while the doctor is going through the provisional license process. As a best practice, it is recommend that states include a “lookback” period of three to five years. This lookback allows a doctor whose license expired shortly after fleeing a country to remain eligible for the licensing pathway.
Practice Experience in Licensing Country
Beyond post-graduate residency, states should require at least a few years of practice to ensure the doctor has sufficient opportunities for patient interaction. Five years of practice after residency or residency equivalent provides the doctor enough time to fully develop their practice and continue honing his skills.
This five-year requirement also protects against a concern that licensing internationally-trained physicians will encourage students in the U.S. to seek a foreign residency. If doctors were eligible for this pathway immediately after residency, medical school graduates might choose exotic and novel residency placements the world over, only to return to the U.S. to practice right away. Requiring doctors to have five years of practice after residency should discourage most American medical students from pursuing this option if their goal is to practice in the United States.
Legally Permitted to Work
To protect both the hiring entity and ensure continuity of care for patients, doctors who follow this pathway should be legally authorized to work in the United States. Many internationally-licensed doctors already live in the United States, including U.S. citizens who studied medicine abroad, green card holders, and refugees. Others will need to apply for a visa to work in the United States legally.
As a best practice, it is recommended that the legislation clearly explain that a sponsoring entity and applicant IMG may apply for the provisional license and that the state medical board may begin its review process and ultimately grant the provisional license, simultaneous with any immigration processes. This would allow a hiring entity and the internationally-licensed doctor to resolve all medical licensing issues while immigration paperwork is pending so that the doctor may begin working in the United States immediately upon the federal government’s decision to give work authorization under federal immigration laws. In such a situation, the provisional license period would not begin until the doctor works in the state.
The Unique State Approaches
Notably, Tennessee was the first state in the recent period to enact legislation that creates a permanent pathway to licensure for internationally-licensed doctors. Bills HB1213 and SB1451 enable doctors who have completed comparable residency training abroad, passed the exams required by the ECFMG, and practiced medicine abroad without incident to enter Tennessee and begin working under the supervision of a hospital or licensed medical facility that already has an accredited residency program in some specialization. The existing residency program can be outside the specialty of the sponsored doctor. This arrangement provides two years of added quality assurance while the doctors integrate into the health system.
In addition to the previously discussed bills from Tennessee, there is palpable momentum nationwide from different states with a strong appetite to utilize the training of specialist doctors from abroad in their states to tackle the physician shortage. The Cicero Institute has compiled the latest from these efforts in different states (Appendix 1).
A snapshot of the efforts in different states highlights a wide variety of legislation that is all moving towards the same goal: addressing physician shortage problems by creating alternative pathways for international physicians rather than taking away residency spots from recent medical school graduates.
Prior to the landmark legislation in Tennessee, Washington passed HB 1129 in 2021, which created a two-year temporary licensure pathway with an option for one renewal but without an option for permanent licensure. Since then, states have developed more and less detailed pathways for full licensure. Colorado, for example, passed HB 1050 in 2022, which shortened the repeat training period for IMGs to gain full licensure from three years to one year and then mandated that the state medical board create a permanent pathway to licensure without repeating residency training. That pathway is still in development.
On the other side of the spectrum, Virginia passed HB 995 in 2024, which creates a two-year provisional license followed by a two-year license restricted to practicing in a rural or underserved community as designated by the Virginia Medical Board. Following this four-year period, doctors can apply for full unrestricted licensure in the state.
Although foreign-trained doctors already contribute significantly to underserved areas in the U.S., matching newly licensed doctors to medically underserved areas may still be challenging.110–111 Currently, areas of physician surplus in the U.S. are often adjacent to medically underserved areas.112 Increasing the number of physicians, therefore, might only go a step toward reducing the physician shortage in medically underserved areas.
The Cicero Institute model legislation (Appendix 2) has formed the foundation for many of these states as they develop their own policy solutions to open the doors of opportunity for internationally-licensed doctors. The model can be customized for the needs on the ground in a particular state.
One customization some states seek to adopt is a rural practice requirement. This requirement (which is now Virginia code) requires IMGs to spend some period of time in a rural or underserved area before the license converts to a full and unrestricted license.
The appetite of health facilities to take up these programs is yet to be seen. Still, given that many health systems are already experienced in organizing visa requirements for IMGs for residency programs and are in need of physicians, they will likely be eager to tap an additional source of highly motivated talent.
As states adopt international physician licensing laws, the facilities and practices that hire foreign doctors will play a key mentorship role in helping to fully integrate these new doctors into the American system of medicine.
One key challenge foreign doctors will still face even if states are willing to grant them a license is how to obtain specialty board certification. Specialty boards are private entities that evaluate and certify the skills of doctors. Some hospitals require specialty board certification for hospital privileges. But the specialty boards, as of this writing, will not grant a certification to a doctor who has not completed medical residency in the United States.113 This is an area of opportunity. Internationally-licensed doctors who join a practice team will have the skills necessary to enter these specialty boards, and the boards should strongly consider creating an alternative pathway to board certification that recognizes the skills and experience an IMG doctor can offer to American patients. As the Federation of State Medical Boards, Accreditation Council of Graduate Medical Education, and Intealth gather their working group on international physician licensing, their collective work on opening specialty board certification opportunities for IMGs would go a long way toward convincing internationally-licensed doctors that they can truly practice in the United States at the top of their training, knowledge, and experience.114
It is essential to look ahead towards other challenges that could come from the influx of foreign doctors at scale. Other countries with a sharp increase in the proportion of foreign nationals in the healthcare workforce include the UK, which has almost 40 percent of the physician workforce coming from foreign countries.115 There is now an emerging body of research from the UK and Australia that can help the U.S. address the potential future challenges of integrating international physicians into the workforce.116–117 Finally, it is worth investigating the underlying dynamics that can lead to a drive for physician recruitment from abroad beyond simply not having enough medical graduates produced domestically. In the UK, for example, there is an exodus of British-trained doctors to other countries that provide better conditions, and it would be prudent for the U.S. to avoid falling into a similar retention crisis.118–119
Finally, as more states consider this policy reform, states, employers, medical boards, and insurance providers will need to gather and analyze data on its benefits, best practices, and lessons learned. Program evaluations of what mechanisms were most effective in reducing physician shortages, the best way to evaluate foreign training and experience, and the ideal kinds of sponsoring entities are all vital topics of continued study in the years ahead.
Conclusion
When Americans call their doctor or visit the hospital, they expect high-quality care delivered by some of the best healthcare professionals in the world. Unfortunately, too many patients are told they must wait weeks or months for an appointment or are seeing their local doctor retire and must travel significant distances to see their replacement.
As America’s population grows and ages and the U.S. physician workforce ages and shrinks, states should embrace creative solutions to address their doctor shortage. Internationally-licensed physicians with experience and high-quality training want to practice medicine in the United States. Still, many are unwilling to endure three or more years of repetitive residency training. States should remove this barrier by allowing healthcare providers to sponsor doctors from around the world for provisional licenses with a pathway to full licensure in the state. States that leverage this new opportunity can protect their patients from the harm ever-growing shortages are creating already and only threaten to worsen in the years ahead. And thanks to the bold leaders who embrace internationally-licensed physicians to close their access gaps, patients can access more care and live happier, healthier lives for many years to come.
Appendix 1: International Physician Bill Status by State
Appendix 2: Model Bill

Stay Informed
Sign up to receive updates about our fight for policies at the state level that restore liberty through transparency and accountability in American governance.
