
2025 State Policy Agenda for Telehealth Innovation
Introduction
While state legislatures remained active in introducing telehealth bills in 2024, significant policy reforms were scarce. Many debates mirrored pre-pandemic discussions, focusing on issues like interstate compacts, insurance coverage mandates, and minor adjustments to existing state laws.
One explanation for this lack of major reforms is that significant telehealth reforms were enacted during the COVID-19 pandemic, potentially reducing the perceived need for further action. This argument could be made for the two of the policy areas this report focuses on: allowing patients to use all kinds of telehealth (modality neutrality), and to start a patient-provider relationship over any mode. Only two states (NC and VT) lack robust and inclusive definitions of the modes of telecare, but 21 would benefit from a few tweaks to get our gold ranking. For starting a relationship over any mode, four states need serious work (AR, KS, TN, and NM), but 12 would benefit from some adjustments.
A relatively small cohort has set the gold standard for the telehealth policy reform of increasing access across state lines to all providers for patients (Arizona, Colorado, Delaware, Florida, Indiana, Louisiana, Utah, and Vermont). Colorado was added to this list in 2024. Most states have defaulted instead to increasing some across-state telehealth access by the far inferior approach of passing compacts (more on this later in the paper).
The battles over independent practice for nurse practitioners still rage in the remaining states that have not expanded in the final policy area of focus for this annual report. The American Medical Association crowed over its lobbying efforts to kill all bills that would have expanded any scope of practice flexibilities in 2024.1
This report should serve as a renewed call for states to update their telehealth laws not to let a patient’s geography determine their health destiny. Telehealth is not a silver bullet, but a basic tool that can be deeply meaningful to the quality of care received by those in rural communities, the disabled, and those with mobility issues.
Telehealth can bring greater efficiency for busy families or any average patient to a healthcare system that desperately needs greater efficiency and more affordable options for patients. It also brings benefits to providers. This report sets a basic policy standard to allow for innovation in care models to emerge, and for patients and providers to have all care options in their toolkits.
New in This Year’s Report: Letter Grades
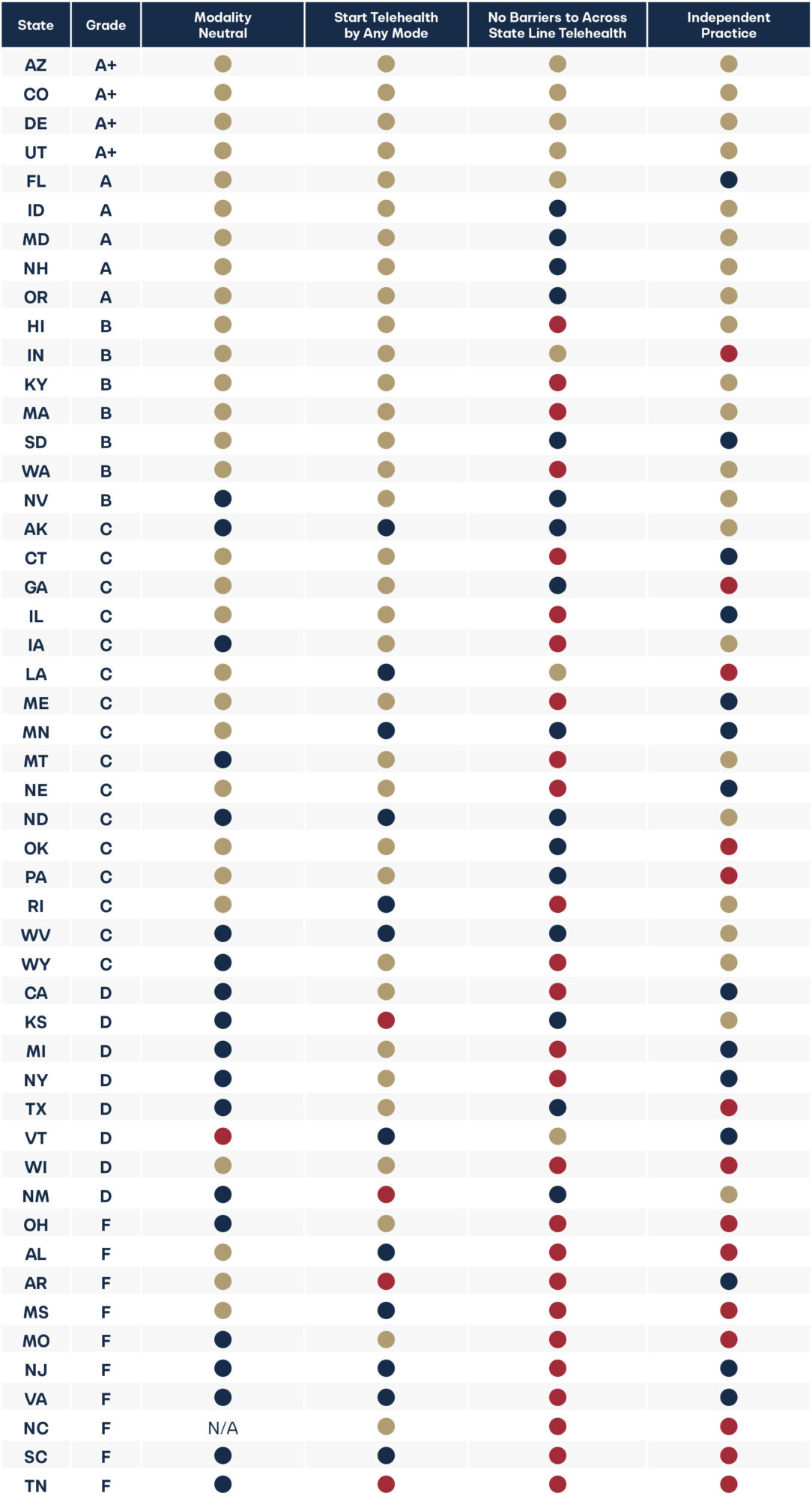
For the first time, this year’s report assigns letter grades to all 50 states. By and large, many states are failing to offer their residents easy access to telehealth of their choice, in or out of state. Only nine states earned an A+ or A grade, seven earned a B, 16 earned a C, eight earned a D, and 10 earned an F. We hope this report will inspire policymakers to improve their grades by helping patients and providers increase access to telehealth options.
State Policy Agenda for Telehealth Innovation and Grades

Methodology for Grades
This report focuses on four key telehealth policy areas: modality-neutral policies, starting a telehealth relationship by any mode, no barriers to across-state-line telehealth, and independent practice for nurse practitioners (all of which are covered in greater depth in the appendix) that impact a patient’s ability to access care. This report examines state telehealth policies for fully-insured private insurance plans and laws that impact provider practice in each state. It does not consider Medicaid policies on telehealth.
To assign the letter grades this year, we used the following method:
For each of the four policy areas, states earned the maximum number of points if their state laws met our gold standard, received half credit if they were in partial compliance (our blue ranking), or zero credit if they were in non-compliance either actively or by omission in their state laws (red ranking).
We gave them all equal value as they are often interconnected for patients. Being able to use live video telehealth is important for some patients, but just as important for ongoing care may be the ability to use remote patient monitoring for a patient being cared for at home, for example. With more and more AI-aided tools hitting the market, being able to start that telehealth relationship and use the best technology available to start a relationship matters. As provider shortages grow, having a more flexible health system will require a health workforce ready to fully leverage technology to meet the health needs of our country. Access to telehealth for patients to all provider types (including nurse practitioners’ independent practices) across state lines is a proxy for a state’s willingness to engage in that discussion.
States Reforms that Changed Rankings
Colorado significantly upgraded their state telehealth laws in 2024 with SB 24-141.2 While implementation is delayed until 2026, the new law passed a registration process for providers in other states to see patients living in Colorado. This law improves its ranking from last year’s red to gold.
Pennsylvania added a formal definition of telemedicine to state law in SB 739, which includes clear outlines of remote patient monitoring, which brings better clarity to companies offering residents all modes of telehealth.3 This improved the states’ ranking from N/A (as they had no definitions) in past years to a gold ranking.
Washington passed SB 5481, which improved the state definitions of telehealth and telemedicine to allow for asynchronous forms.4 Previously state law had required a real-time mandate, which did not allow patients to start the relationship in the mode they preferred. This improves its ranking from blue to gold for modality neutral and starting the telehealth relationship. The state could still benefit from adding a definition for remote patient monitoring to reach gold status.
Reforms That Missed the Mark
Alaska: SB 91 explicitly allowed members from out of state to join a multidisciplinary team in Alaska over telehealth.5 However, the new law kept barriers in place to prevent these out-of-state providers from seeing patients outside of that team. This change is not that different from other states that allow consultations over telehealth and is not enough to improve Alaska’s ranking for no barriers to across-state-line telehealth.
Connecticut: HB 5198 added a registration pathway for across-state-line telehealth but also added barriers to access by requiring that an out-of-state provider must engage with or contract with an in-state entity or provider before offering telehealth.6 This arrangement is not very different from other states that place restrictions on across-state-line care by only allowing consultations or temporary care, so it does not change their ranking from red. The law also allows the Commissioner of Public Health 45 days to approve every application, which adds a potential delay and barrier to care.
Louisiana: After improvements last session to require their boards to allow across-state-line access for patients, a concerning small step backward may have passed in SB 66, which mandates that telehealth visits must make referrals to in-state providers or arrange follow-up care in-state as necessary.7 The interpretation of “as necessary” will determine how strict this mandate turns out to be for patients. This may threaten their current gold-standard ranking.
Tennessee: SB 18818/HB2957 made the outlier state requirement of having to see a provider within the last 16 months before a provider can see a patient over telehealth worse by now requiring it before any telehealth visit. This is a further step backwards for patients and changes the state’s ranking from gold to red for starting a relationship by any mode. This last-minute change to the original bill resulted in the American Telemedicine Association’s advocacy arm withdrawing its support for the bill.9
Washington: Even with the improvements in Washington noted above, the state missed the mark on changes to across-state-line telehealth access. The new law added pathways for providers out-of-state to see patients but kept them limited to consultations and followup care or mental health services for a short period of time. This was not enough to change our ranking.
Compacts Have Severe Limits
Of the 52 enacted bills that impacted across-state-line access, 35 were compacts—almost 70 percent. Twelve states passed the new social worker compact alone. If those states had passed a simple registration bill, patients in their states could access all provider types now, not just one or two for those covered by the new compact, and many of the new compacts, like the social worker compact, are years away from being up and running.
As we covered in past years’ reports, compacts have severe limitations.
These include:
- They Are Slow
To get passed, to get set up, and to get approved for the provider (depending on the compact). - They Are Expensive
To get passed, to get set up, and for the providers to take part. - They Impact Fewer States
Limited only to providers in compact states. - They Are Too Narrow
Limited to one kind of provider type covered by that specific compact.
States are being short-sighted by focusing so much time and so many resources on passing compacts. Instead, they could pass one bill that sets up a streamlined registration process for all providers so that patients in their states could have these new options right away instead of waiting until the care they need gets a provider compact (as many providers don’t have a compact for their area of focus), and high-priced lobbyists get paid to get that compact passed.
Appendix 1. Policy Areas Covered in This Report
Modality Neutral
A quality-oriented, provider and patient-centered health system means allowing for many kinds of telehealth, not just live video. For this category, the report largely follows the term as defined by the American Telemedicine Association (ATA) which points to a “modality-neutral” definition of telehealth including various methods whether asynchronous or synchronous, and various technologies whether by audio-video, store-and-forward, or remote patient monitoring.
“Telehealth” means a mode of delivering healthcare services using telecommunication technologies, including but not limited to asynchronous and synchronous technology, and remote patient monitoring technology by a healthcare practitioner to a patient or a practitioner at a different physical location than the healthcare practitioner.
Remote patient monitoring refers to the transmission and monitoring of personal health data (including vital signs, weight, blood pressure, blood sugar, blood oxygen levels, heart rate, and electrocardiograms) via electronic communication technologies. Remote patient monitoring allows providers to track a patient’s health data outside of a facility. This is beneficial for preventing readmissions and allowing older adults and individuals with disabilities to live at home and avoid admission into a skilled nursing facility.
Store-and-forward refers to the electronic transmission of digital medical information including prerecorded video or images (such as X-rays, MRIs, or photos of skin conditions). Store-and-forward transfers are particularly useful for consultations with specialists who can review medical information after it has been collected and uploaded. This provides patients access to specialty care promptly without the need for coordinating schedules and lengthy travel.
Start Telehealth by Any Mode
Every patient has their own preference for how to interact with a healthcare provider. As a result, allowing flexibility for the relationship to be initiated through the patient’s preferred modality—when the standard of care can be met—is imperative. Imagine someone experiencing a behavioral health crisis in the middle of the night. They might strongly prefer to start communication by text or in an asynchronous manner before being comfortable switching to a video call or in-person visit. Providers should be able to accommodate that preference so long as the standard of care can be met. If the nation’s healthcare system is going to be more patient-centered and accessible while taking care to avoid wasting money, state laws need to ensure these better methods to deliver care are available. Some states allow for the use of both synchronous and asynchronous modalities but may limit the modalities that a provider may use to form the relationship—regardless of what is clinically appropriate. That is what is being ranked here. Laws and board regulations should remove barriers that get in the way of forming a telehealth relationship.
No Barriers for Patients to Across-State-Line Telehealth
Allowing patients to access providers outside their community is imperative as most cities and towns simply lack certain kinds of providers. Telehealth may be their only option for seeing a specialist, getting a second opinion, or accessing team-based care. Allowing across-state-line telehealth ends geographic and economic discrimination for many patients and allows access to providers who would not otherwise be accessible due to distance or the expense of travel.
Too many states and medical boards have made it time-consuming and expensive to see patients outside their home state Others have prohibited it entirely. Pilots don’t lose their skills when they cross a state line, and neither do healthcare professionals. As Americans become increasingly mobile, being able to stay in touch with providers who know the patient’s history and have their trust is imperative to better health outcomes.
This category highlights states that allow providers in good standing to see patients in another state without jumping through expensive time-consuming hoops—and not just for a consultation with another provider or during an emergency. States that earned a positive ranking often allowed providers to register to see new patients or provide simple reciprocity for providers in good standing. Anything over and above these requirements are barriers to the provider-patient relationship, and many of the provider compacts being pushed have severe, unnecessary limitations.
Imagine that a family member gets sick and the nation’s leading expert on treating the illness works at the Cleveland Clinic in Ohio, where you don’t live. If you are wealthy, you could travel to Ohio and pay out of pocket for the services. If you are middle-class or low-income, you have no such option. Your family member could not see this specialist unless they convinced the provider to go through the time and expense of obtaining a full medical license in their state. This is discrimination by geography and economic status. Telehealth reform is a market-based equalizer.
Previous research from the Cicero Institute has shown few there are disciplinary problems for across-state-line telehealth, making it a safe and smart solution.
Independent Practice
The report rates each state based on whether nurse practitioners (NPs) are allowed to practice as they have been trained, or if the state still requires a doctor to provide oversight or co-sign their work.
The U.S. has an acute shortage of doctors that is projected to grow in the years to come. Expanding the supply of healthcare professionals with high-quality nurse practitioners is not only a prudent option, it is a necessity. It increases practitioner access for patients while allowing doctors to focus on the most complex cases and sickest patients. Ample research has shown that expanding NPs’ scope of practice increases access to care and reduces costs without compromising quality. Absent reform, many patients may be forced to go without care.
It is important to acknowledge that expanding the scope of practice for pharmacists, physician assistants, dentists, and other medical providers can also be important as well. However, because of the impact of NPs being allowed to practice independently on patient access, this was the focus of the report.
Appendix 2. State Innovation Policies Updated Needed
| State | Modality Neutral | Start Telehealth by Any Mode | No Barriers to Across-State-Line Telehealth | Independent Practice |
|---|---|---|---|---|
| AK | Add a definition for remote patient monitoring or store-and-forward technologies. | Remove standard that it is considered unprofessional conduct if providing treatment, rendering a diagnosis, or prescribing medications based solely on a patient-supplied history that a physician licensed in this state received by telephone, facsimile, or electronic format. This puts in place a barrier to patients starting a relationship in the mode they prefer. | Amend or replace the Alaska business license requirement for telehealth providers to allow for an easy registration or reciprocity law for all providers. Alternatively, allow all providers on a multi-disciplinary team to see patients independently as passed in SB 91. | N/A |
| AR | N/A | Update Medical Board regulations that require a face-to-face examination using real-time technology, and forwarded medical histories to establish a patient-provider relationship. These rules limit patient choice to start a relationship in an asynchronous manner. | Pass an easy registration or reciprocity law for all providers. | Remove the collaborative practice agreement mandate of 6,240 hours before NPs can practice independently. |
| AZ | N/A | Amend Medical Practice Act to remove restrictions on prescribing by providers to only those with an established doctor-patient relationship or those who conduct an examination during a real-time telemedicine encounter with audio and video capability. This places a barrier to patient access to the provider that is the best fit for their care. | N/A | N/A |
| CA | Add a definition for remote patient monitoring. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove 4,600-hour supervision mandate. |
| CO | N/A | N/A | N/A | It would not impact the ranking, but an additional suggestion is to eliminate the mandated transition period for prescription authority. |
| CT | N/A | N/A | Eliminate requirement that providers must engage with or contract with an in-state provider or entity before seeing a patient in the state. Remove the Commissioner of Public Health approval step of each application, making it automatic if the provider meets certain criteria. | Remove three-year supervision mandate. |
| DE | N/A | Amend the Medical Practice Act to remove real-time modality. | N/A | N/A |
| FL | N/A | N/A | Should remove prohibition on registered telehealth providers from providing in-state care. | Remove 3,000-hour supervision mandate. |
| GA | N/A | Make it clear that a patient-provider relationship can start over any mode. | Expand special telemedicine licenses for physicians to all providers from other states in good standing. | Allow NPs to practice independently. |
| HI | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | N/A |
| IA | Add definition for remote patient monitoring and store-and-forward into state law, remove interactive requirement. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | N/A |
| ID | N/A | N/A | Expand the across-state-line option opened for behavioral health to all provider types. | N/A |
| IL | N/A | Remove established patient requirement that blocks some patient access to starting a relationship. | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently by removing the transitional collaborative practice agreement mandate of 4,000 hours and 250 hours of continuing education. |
| IN | N/A | N/A | N/A | Allow NPs to practice independently. |
| KS | Remove real-time requirement in the definition of telemedicine, and add definition for remote patient monitoring. | Make it clear that a patient-provider relationship can start over any mode. | Expand telemedicine waiver in law that currently only applies to the 16 professions regulated by the Kansas State Board of Health Arts to apply to all providers. This may require a broadening of the definition of healthcare provider in the statute. | N/A |
| KY | Add a definition for store-and-forward. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove four-year practice requirement before being allowed to prescribe. |
| LA | N/A | Make it clear that a patient-provider relationship can start over any mode which will lead to changes to the Board of Medical Examiners regulations that raise doubt that a patient can start a relationship by asynchronous telemedicine. | Make it clear that referrals to in-state providers are not mandated but should follow the normal standard of care if necessary. This would avoid confusion that could be caused by SB 66 that no follow up care is permitted by out-of-state providers. | Allow NPs to practice independently. |
| MA | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | Remove two years of experience before allowed to prescribe. |
| MD | Remove the interactive requirement in the insurance code. | N/A | Pass an easy registration or reciprocity law for all providers that extends beyond just the narrow list currently allowed for physicians. | N/A |
| ME | N/A | Make it clear that a patient-provider relationship can start over any mode. | Remove physician consultation limitation for across-state-line care, and pass an easy registration or reciprocity law for all providers. | Remove 24-month supervision mandate. |
| MI | Add definition for remote patient monitoring. It exists for Medicaid in the state but not the private market. | N/A | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently without a delegation requirement for certain kinds of prescribing and for Medicaid reimbursement. |
| MN | Update current law that defines telehealth as having to be a real-time, two-way interactive audio and visual communication, but also allows store-and-forward options. This can cause confusion. | Make it clear that a patient-provider relationship can start over any mode. | Expand the physician across-state-line registration or a reciprocity law to all providers. | Remove 2,080-hour collaborative practice agreement mandate. |
| MO | Remove the interactive requirement in the insurance code and define remote patient monitoring. | N/A | Pass an easy registration or reciprocity law for all providers that extends beyond the narrow list currently allowed for physicians. | N/A |
| MS | The state definition includes store-and-forward and remote patient monitoring, but mandates everything else be real-time audio video, unless the Commissioner of Insurance allows other situations without that. Update the definition to remove any real-time requirement. Remove the sunset in 2025. | Fixing the definition list in column one would make it clear that any mode is accepted to start a provider-patient relationship. Board of Medical Licensure regulations need to be fixed to remove requirements of telehealth being capable of replicating an in-person visit, as that prevents a patient-provider relationship from being established through asynchronous telehealth. | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently. |
| MT | Add definition for remote patient monitoring. | N/A | Pass an easy registration or reciprocity law for all providers. | N/A |
| NC | Add robust definitions for telehealth. A law this year added the definition that appears only to apply for mental health, and was tied to disaster assistance and recovery. Building out these definitions to more standard language would bring clarity. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove collaborative agreement mandate. |
| ND | Add a definition for telehealth that mentions remote patient monitoring. | Make it clear that a patient-provider relationship can start over any mode. Remove in-person medical evaluation in the North Dakota Food, Drug and Cosmetic Act. | Expand on license by endorsement that only applies to physicians and physician assistants to apply a reciprocity or easy registration to all providers in good standing. | N/A |
| NE | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | Remove 2,000-hour supervision mandate. |
| NH | N/A | N/A | Build on the reciprocity law for physicians and physician assistants to include all providers and put in place an easy registration process for telehealth services. Or expand tele-pass for psychologists to all providers. | N/A |
| NJ | Remove any remaining references in regulation for real-time or video-only telehealth. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | End collaborative agreement mandate for prescribing. |
| NM | Remove interactive requirement. | Update regulations that require face-to-face telehealth visits. And allow prescribing without face-to-face encounters. | Streamline special telemedicine license for doctors, and pass an easy registration or reciprocity law for all providers. | N/A |
| NV | Add definition for remote patient monitoring. | N/A | Streamline Board of Medical Examiners optional special purpose licenses to a registration. Pass an easy registration or reciprocity law for all providers. | Remove two years or 2,000-hour requirement before being able to prescribe controlled substances. |
| NY | Add definition for remote patient monitoring or store-and-forward telehealth. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove collaboration mandate. Remove collaboration mandate, and 3,600 hours of practice requirement before allowing independent practice. |
| OH | Add a definition for telehealth that mentions store-and-forward, and remote patient monitoring. | N/A | Pass an easy registration or reciprocity law for all providers. | Remove collaborative agreement mandate and let NPs practice independently. |
| OK | N/A | N/A | Pass an easy registration or reciprocity law for all providers that moves beyond the subjective process only extended by the Board of Osteopathic Examiners. | Remove supervision mandate and collaborative agreement mandate. |
| OR | N/A | It would not impact the ranking, but it would be helpful to make it clear that a provider-patient relationship can be started by an online form when appropriate. | Pass an easy registration or reciprocity law for all providers that moves beyond the subjective process only extended to physicians (MD/DO), podiatric physicians, and physician assistants. | N/A |
| PA | Add a definition for store-and-forward. | N/A | Pass an easy registration or reciprocity law for all providers that extends beyond just the providers from adjoining states. | Remove collaborative agreement mandate and let NPs practice independently. |
| RI | Remove reference in regulation (216-RICR-40-05-1) that states that asynchronous evaluation of a patient, without contemporaneous real-time, interactive exchange between the physician and patient, is not appropriate. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | N/A |
| SC | Add definitions for remote patient monitoring and store-and-forward in the provider code. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. Don’t require providers living out of the state still to obtain a South Carolina full license. | Remove the written protocol requirement. |
| SD | N/A | N/A | Pass an easy registration or reciprocity law for all providers, and make the physician pathway automatic if they are in good standing. | Remove 1,040-hour practice mandate before being allowed to practice independently. |
| TN | Remove prohibition of remote patient monitoring for provider-based telemedicine. Add definition of remote patient monitoring. | Remove requirement that for provider-based telemedicine there has to be proof of an in-person encounter and an insurance claim. TN and WV are the only states with this out-of-date requirement. Remove requirement that for a patient to receive telehealth they must be at a qualified site such as a school, and that providers must have access to the patient’s medical record. | Pass an easy registration or reciprocity law for all providers, building on subjective process now only for physicians and osteopathic physicians. | Allow NPs to practice independently. |
| TX | Add definitions for remote patient monitoring and store-and-forward. | N/A | Streamline across-state-line pathway for physicians to just a registration or none. Add universal pathway for all other providers in good standing. | Allow NPs to practice independently. |
| UT | N/A | Allow the provider-patient relationship to be formed using online options, including for prescriptions. | N/A | N/A |
| VA | Add formal definitions outside of the statewide telehealth plan for remote patient monitoring and store-and-forward. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove five-year practice requirement before allowing independent practice. |
| VT | Remove the live requirement for telemedicine. Add definition for remote patient monitoring. Remove requirement for an image for store-and-forward communication. | Make it clear that a patient-provider relationship can start over any mode. | State should expand the across-state-line license and registration to all provider types, and remove the patient limit and prohibition of care in the state. | Remove the 2,400-hour or two-year collaborative agreement mandate. |
| WA | N/A | N/A | Pass an easy registration or reciprocity law for all providers. Expand the pathway passed in SB 5481. | N/A |
| WI | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently. |
| WV | Add definition for store-and-forward. Remove established patient category to remove face-to-face requirement. | Remove interactive and real-time requirements to establish a patient-provider relationship. | Remove prohibition from seeing a patient in state, and allow patients to see across-state-line physicians from other states without requiring them to first be licensed in West Virginia. | Remove three-year collaborative agreement mandate for prescribing. |
| WY | Add a uniform definition for telehealth that makes it clear that synchronous, asynchronous, remote patient monitoring and store-and-forward are allowed. | N/A | Pass an easy registration or reciprocity law for all providers. | N/A |

Stay Informed
Sign up to receive updates about our fight for policies at the state level that restore liberty through transparency and accountability in American governance.
