
2024 State Policy Agenda for Telehealth Innovation
Introduction
In 2023, state legislative progress on reforming telehealth laws stalled, with a few exceptions. Even as many public health emergency declarations for COVID-19 expired in 2023, state legislation did not keep pace with the momentum to maintain the greatest flexibilities granted under those declarations.
Three states (Idaho, Louisiana, and Utah) deserve special recognition for the largest telehealth policy updates passed in 2023. Other states should take notice and copy their reforms.
This is the third annual 50-state telehealth innovation report card that captures innovation-minded telehealth policy changes that took place this past year.1 At the 30,000-foot level, the telehealth policy reforms that did pass in 2023 can be characterized as largely tweaking around the edges. Many of the telehealth bills filed around the country fell into the familiar areas pushed by special interests to mandate coverage of certain services, or mandating certain payment levels. Few bills focused on making the telehealth landscape flexible enough to allow for innovation.
While news stories of average Americans highlighted the many cost and access challenges that patients routinely face to receive care, most states failed to move the needle on telehealth reform to ease some of that tension. Most patients still lack electronic access to providers outside of their state, even if there are few or no providers of a specific type near them. If we did this for pilots, almost no one could access or afford an airplane ticket. Yet that has been our approach for medical providers.
A new study released in early 2023, “Few Disciplinary Issues with Out-of-State Telehealth: New Data from Florida and Idaho,” co-authored by one of this report’s co-authors and Dr. Ateev Mehrotra of Harvard Medical School found that providers are increasingly interested in offering their expertise to patients in states that allow such a framework, and there had been no disciplinary action taken against those providers over hundreds of thousands of visits. Yet only Louisiana and Utah made moves in 2023 towards opening up these options, with Idaho doing so for behavioral health.
There was some movement on compacts that can impact telehealth access, but compacts are not the most flexible. Two states (Hawaii and Missouri) joined the Interstate Medical Licensure Compact. Indiana joined the counseling compact, and Louisiana joined the occupational therapy compact. Yet compacts only apply to one kind of provider, only apply among mutual compact states, and have faced criticism for still being slow to approve across-state line access and include a decent cost to do so.
This toolkit is designed to guide policymakers in advancing a healthcare system that prioritizes quality, affordability, and innovation. Its primary goal is to assist state governments in revising telehealth laws to eliminate historical barriers that have disproportionately affected certain individuals in specific regions.
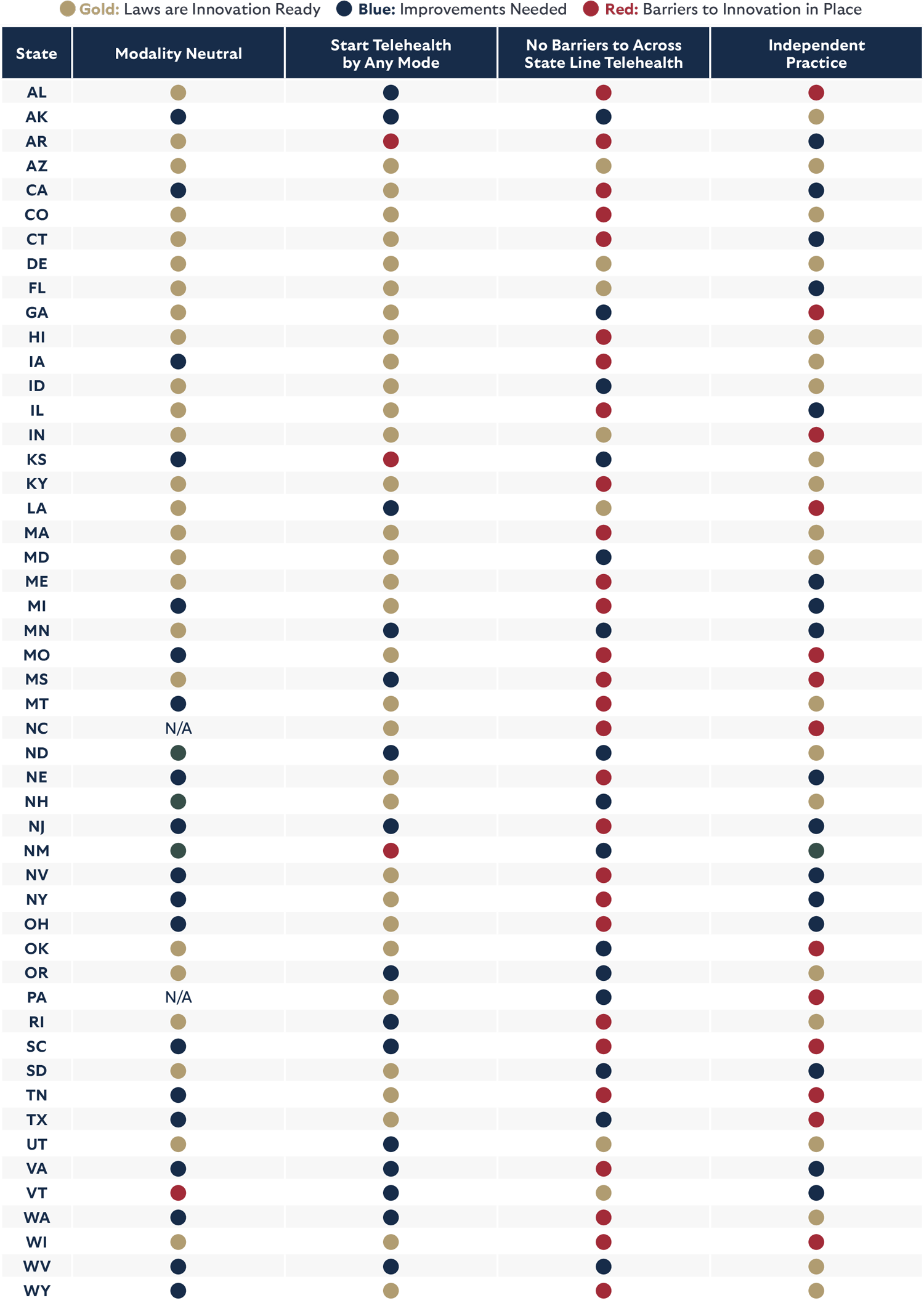
The following report outlines policy best practices to optimize the benefits of telehealth services for providers and patients. Additionally, it includes a straightforward stoplight rating system for each state, indicating the alignment of their policies with the identified best practices. The appendix offers specific changes that are needed in each state to improve its rankings.
Urgent action is imperative for states to meet the physical and economic needs of their residents through a forward-thinking and quality-oriented healthcare system.
State Policy Agenda for Telehealth Innovation
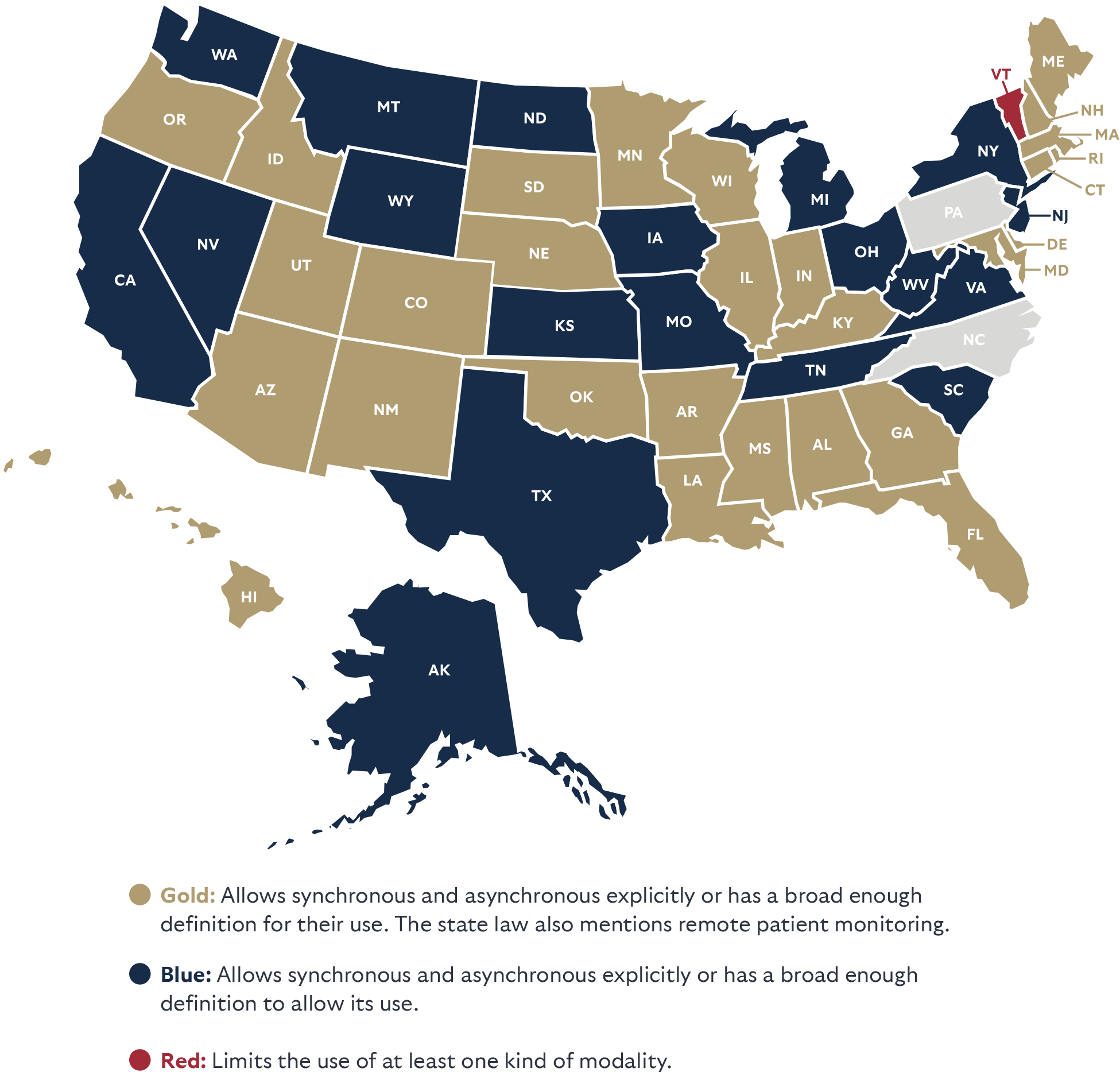
Modality Neutral
A quality-oriented, provider and patient-centered health system means allowing for many kinds of telehealth, not just live video. For this category, the report largely follows the term as defined by the American Telemedicine Association (ATA) which points to a “modality-neutral” definition of telehealth including various methods whether asynchronous or synchronous, and various technologies whether by audio-video, store and forward, or remote patient monitoring.
“Telehealth” means a mode of delivering healthcare services using telecommunication technologies, including but not limited to asynchronous and synchronous technology, and remote patient monitoring technology, by a healthcare practitioner to a patient or a practitioner at a different physical location than the healthcare practitioner.
Remote patient monitoring refers to the transmission and monitoring of personal health data (including vital signs, weight, blood pressure, blood sugar, blood oxygen levels, heart rate, and electrocardiograms) via electronic communication technologies. Remote patient monitoring allows providers to track a patient’s health data outside of a facility. This is beneficial for preventing readmissions and allowing older adults and individuals with disabilities to live at home and avoid admission into a skilled nursing facility.
Store-and-forward refers to the electronic transmission of digital medical information including prerecorded video or images (such as X-rays, MRIs, or photos of skin conditions). Store-and-forward transfers are particularly useful for consultations with specialists who can review medical information after it has been collected and uploaded. This provides patients access to specialty care promptly without the need for coordinating schedules and lengthy travel.
STATE HIGHLIGHT: UTAH
Utah passed one of the most promising across-state line telehealth reform law (HB 159) this past year. The reform moves Utah’s stoplight chart ranking from blue to gold. The state now has a predictable and streamlined application process to offer patients additional access to care. Utah created an automatic “nonresident healthcare license” and if a provider’s application is not processed within 15 days of being submitted, it is considered automatically approved as long as the applicant does not violate any other state laws. The trigger of a 15-day processing timeline provides predictability that most other state laws do not have. It will be interesting to monitor how long it takes the provider boards issuing these licenses to process any new applications, and how many are approved because they exceed this 15-day window.
STATE LAWS ON ALLOWING MANY METHODS
FOR PATIENTS TO ACCESS TELEHEALTH
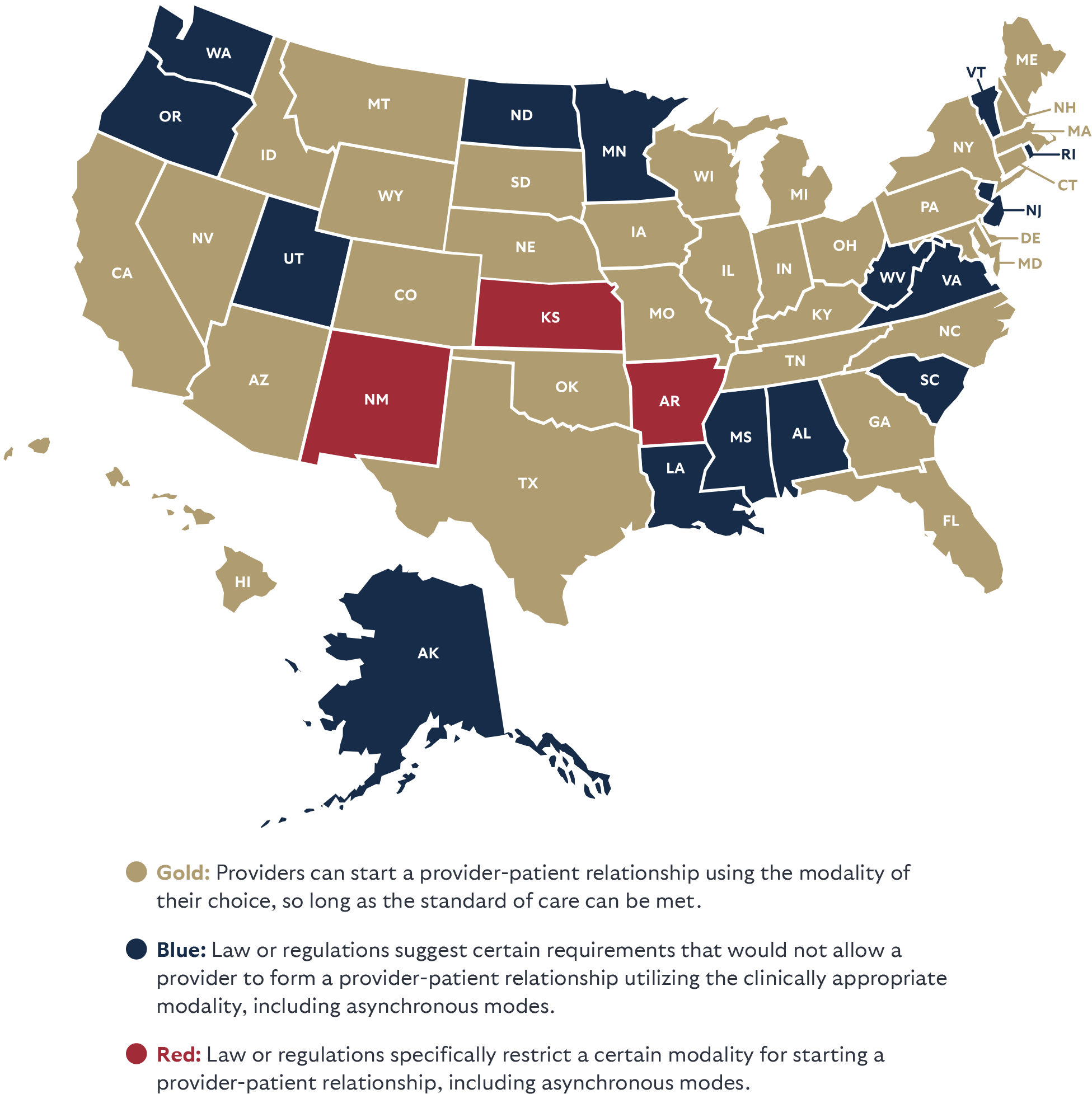
Start Telehealth by Any Mode
Every patient has a different preference for how to interact with a healthcare provider. As a result, allowing flexibility for the relationship to be initiated through the patient’s preferred modality—when the standard of care can be met—is imperative. Imagine someone experiencing a behavioral health crisis in the middle of the night. They might strongly prefer to start communication by text or in an asynchronous manner before being comfortable switching to a video call or in-person visit, and providers should be able to accommodate that preference so long as the standard of care can be met. If the nation’s healthcare system is going to be more patient-centered, accessible, and avoid wasting money—then state laws need to ensure these better methods to deliver care are available. Some states allow for the use of both synchronous and asynchronous modalities (as highlighted in the map) but may limit the modalities that a provider may use to form the relationship—regardless of what is clinically appropriate—which is what is being ranked here. Laws and board regulations should remove barriers that get in the way of forming a telehealth relationship.
STATE HIGHLIGHT: IDAHO
Idaho passed a few new telehealth laws this past year. The state also updated its laws to allow a provider to start a provider-patient relationship using asynchronous telehealth so long as the standard of care can be met, which changes their stoplight ranking from red to gold on this front. Another new law (HB 61) allows for across-state line care for behavioral health. This change moves Idaho’s stoplight chart ranking from red to blue.
STATE LAWS ON PATIENTS STARTING A RELATIONSHIP
BY ANY MODE OF TELEHEALTH
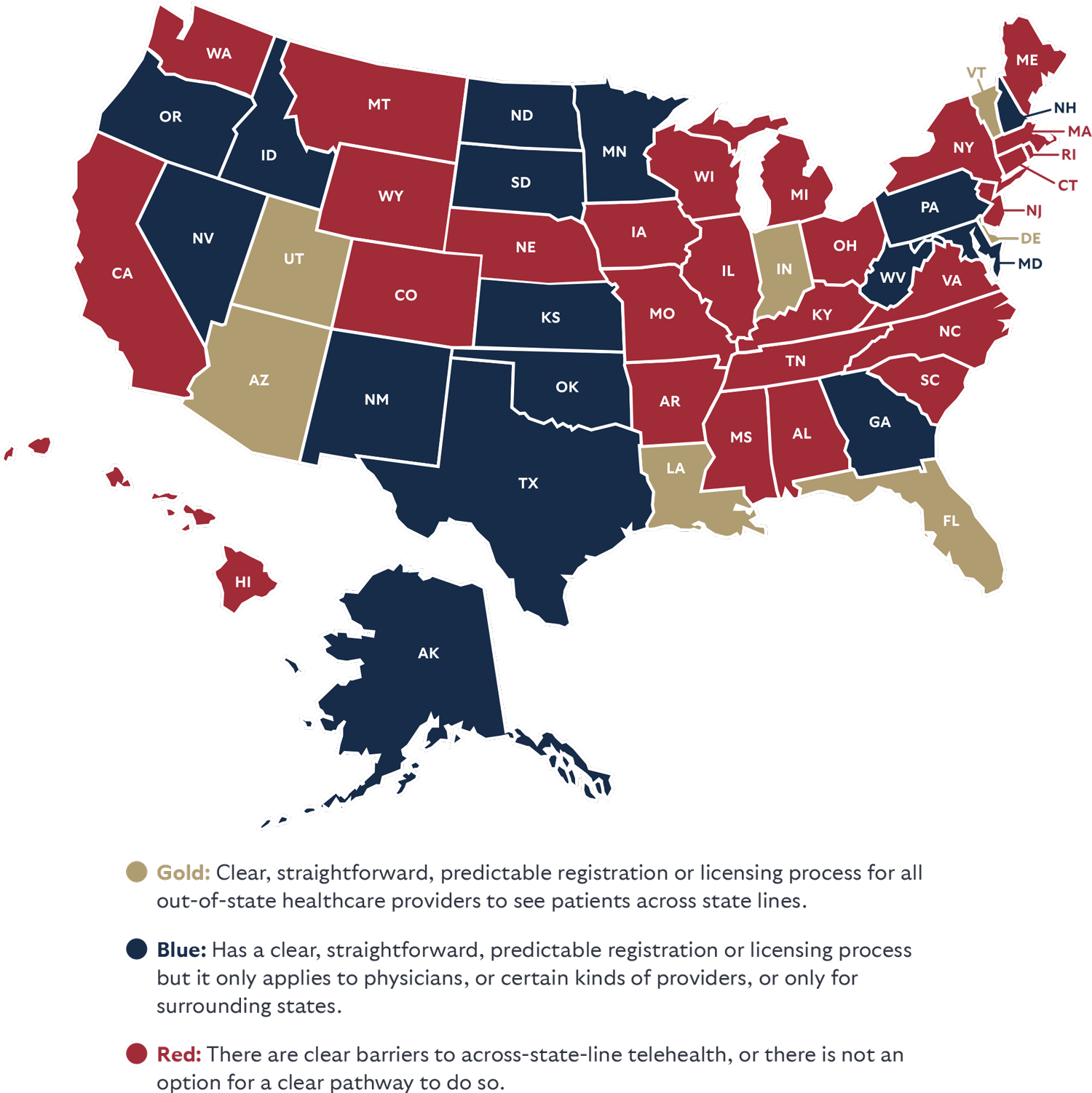
No Barriers for Patients to Across State Line Telehealth
Allowing patients to access providers outside their community is imperative as most cities and towns simply lack certain kinds of providers.2 Telehealth may be their only option for seeing a specialist, to get a second opinion or access team-based care. Allowing across-state-line telehealth ends geographic and economic discrimination for many patients and allows access to providers who would not otherwise be accessible by distance or expense of travel.3
Too many states and medical boards have made it time-consuming, expensive, or prohibited providers from seeing patients outside their home state. Pilots don’t lose their skills when they cross a state line, and neither do healthcare professionals. As more Americans are mobile, being able to stay in touch with providers who know the patient’s history and have their trust is imperative to better health outcomes.
This category highlights states that allow providers in good standing to see patients in another state without jumping through expensive time-consuming hoops—and not just for a consultation with another provider or during an emergency. States that earned a positive ranking often allowed providers to register to see new patients or provide simple reciprocity for providers in good standing. Anything over and above these requirements are barriers to the provider-patient relationship, and many of the provider compacts being pushed have severe limitations.
Imagine that a family member gets sick and the nation’s leading expert on treating the illness works at the Cleveland Clinic in Ohio, where you don’t live. You could not see this specialist unless you convinced the provider to go through the time and expense of obtaining a full medical license in your state. If you are wealthy, you could travel to Ohio and pay out of pocket for the services. Middle-class and low-income residents have no such option. This is discrimination by geography and economic status. Telehealth reform is a market-based equalizer.
STATE HIGHLIGHT: LOUISIANA
Louisiana took a big step to modernize its telehealth laws (SB 66) by standardizing their definitions and requiring their licensing boards to promulgate rules for interstate registration. Prior state law had only encouraged the boards to issue rules around interstate telehealth. Unsurprisingly, very few boards allowed interstate registration under the old language. The specific word change needed to update the state laws was called for by one of the co-authors of this report in a 2021 report in Louisiana.
STATE LAWS THAT DON’T REQUIRE SICK PATIENTS TO TRAVEL TO ACCESS PROVIDERS IN ANOTHER STATE
Independent Practice
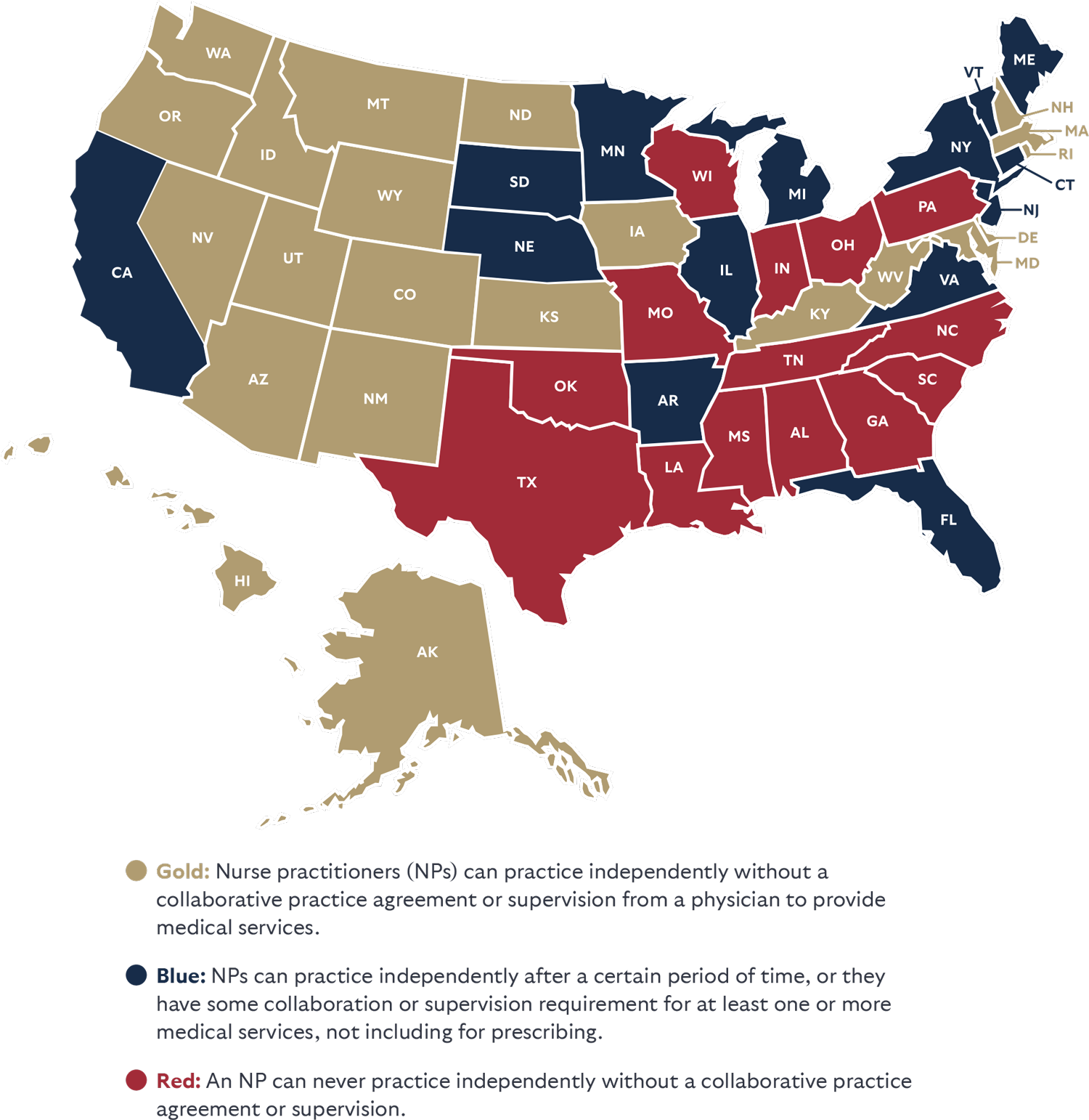
The report rates each state based on whether nurse practitioners (NPs) are allowed to practice in the way they have been trained, or if the state still requires a doctor to provide oversight or co-sign their work.
The country has an acute shortage of doctors that is projected to grow to up to 124,000 by 2034.4 Expanding the supply of healthcare professionals with high-quality nurse practitioners is not only a nice option to have for patients, but a necessity. It also allows doctors to focus on the most complex and sick patients. Ample research has shown that expanding NPs’ scope of practice increases access to care and reduces costs without compromising quality.5 Absent reform, many patients may be forced to go without care.
It is important to acknowledge that expanding the scope of practice for pharmacists, physician assistants, dentists, and other medical providers can also be important as well. Because of the impact of NPs being allowed to practice independently on patient access, this was the focus of the report.
STATE LAW ON HAVING MORE PROVIDER OPTIONS
Appendix: State Innovation Policy Updates Needed
| State | Modality Neutral | Start Telehealth by Any Mode | No Barriers to Across State Line Telehealth | Independent Practice |
|---|---|---|---|---|
| AL | Add robust definitions for telehealth. | Make it clear that a patient-provider relationship can start over any mode. | Replace limited special purpose license for just doctors and replace it with an easy registration or reciprocity law for all providers. | Allow NPs to practice independently. |
| AK | Add definition for remote patient monitoring or store-and-forward technologies. | Remove standard that it is considered unprofessional conduct if providing treatment, rendering a diagnosis, or prescribing medications based solely on a patient-supplied history that a physician licensed in this state received by telephone, facsimile, or electronic format. This puts in place a barrier to patients starting a relationship in the mode they prefer. | Amend or replace the Alaska business license requirement for telehealth providers to allow for an easy registration or reciprocity law for all providers. | N/A |
| AR | N/A | Update Medical Board regulations that require a face-to-face examination using real time technology, and forwarded medical histories to establish a patient-provider relationship. These rules limit patient choice to start a relationship in an asynchronous manner. | Pass an easy registration or reciprocity law for all providers. | Remove collaborative practice agreement mandate of 6,240 hours before NPs can practice independently. |
| AZ | N/A | Amend Medical Practice Act to remove restrictions on prescribing by providers to only those with an established doctor-patient relationship or those who conduct an examination during a real-time telemedicine encounter with audio and video capability. This places a barrier to patient access to the provider that is the best fit for their care. | N/A | N/A |
| CA | Add a definition for remote patient monitoring. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove 4,600-hour supervision mandate. |
| CO | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | Updated to reflect state law, but the state could eliminate a mandated transition period for prescription authority. |
| CT | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | Remove three-year supervision mandate. |
| DE | N/A | Amend the Medical Practice Act to remove real-time modality. | N/A | N/A |
| FL | N/A | N/A | Should remove prohibition on registered telehealth providers from providing in state care. | Remove 3,000-hour supervision mandate. |
| GA | N/A | Make it clear that a patient-provider relationship can start over any mode. | Expand special telemedicine license for physicians to all providers from other states in good standing. | Allow NPs to practice independently. |
| HI | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | N/A |
| IA | Add definition for remote patient monitoring and store-and-forward into state law, remove interactive requirement. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | N/A |
| ID | N/A | N/A | Expand the across-state-line option opened for behavioral health to all provider types. | N/A |
| IL | N/A | Remove established patient requirement that blocks some patient access to starting a relationship. | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently by removing the transitional collaborative practice agreement mandate of 4,000 hours and 250 hours of continuing education. |
| IN | N/A | N/A | N/A | Allow NPs to practice independently. |
| KS | Remove real-time requirement in the definition of telemedicine, and add definition for remote patient monitoring. | Make it clear that a patient-provider relationship can start over any mode. | Expand telemedicine waiver in law that currently only applies to the 16 professions regulated by the Kansas State Board of Health Arts, to all providers. This may require a broadening of the definition of healthcare provider in the statute. | N/A |
| KY | Add a definition for store-and-forward. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove four-year practice requirement before being allowed to prescribe. |
| LA | N/A | Make it clear that a patient-provider relationship can start over any mode which will lead to changes to the Board of Medical Examiners regulations that raise doubt that a patient can start a relationship by asynchronous telemedicine. | A review of updated regulations next year will be required to ensure full flexibility. | Allow NPs to practice independently. |
| MA | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | Remove two years of experience before allowed to prescribe. |
| MD | Remove the interactive requirement in the insurance code. | N/A | Pass an easy registration or reciprocity law for all providers that extends beyond just the narrow list currently allowed for physicians. | N/A |
| ME | N/A | Make it clear that a patient-provider relationship can start over any mode. | Remove physician consultation limitation for across-state-line care, and pass an easy registration or reciprocity law for all providers. | Remove 24-month supervision mandate. |
| MI | Add definition for remote patient monitoring. | N/A | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently without a delegation requirement for certain kinds of prescribing and for Medicaid reimbursement . |
| MN | Update current law that defines telehealth as both having to be a real-time two-way interactive audio and visual communication, but also allows store-and-forward options. This can cause confusion. | Make it clear that a patient-provider relationship can start over any mode. | Expand the physician across-state-line registration or a reciprocity law to all providers. | Remove 2,080-hour collaborative practice agreement mandate. |
| MO | Remove the interactive requirement in the insurance code and define remote patient monitoring. | N/A | Pass an easy registration or reciprocity law for all providers that extends beyond just the narrow list currently allowed for physicians. | N/A |
| MS | New law (SB 2738) definition includes store-and-forward and remote patient monitoring, but mandated everything else be real-time audio video, unless the Commissioner of Insurance allows other situation without that. Update the definition to remove any real-time requirement. Remove the sunset in 2025. | Fix to definition list in column 1 would make it clear that any mode is accepted to start a provider-patient relationship, but Board of Medical Licensure regulations need to be fixed to remove requirements of telehealth being capable of replicating an in-person visit, as that prevents a patient-provider relationship from being established through asynchronous telehealth. | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently. |
| MT | Add definition for remote patient monitoring. | N/A | Pass an easy registration or reciprocity law for all providers. | N/A |
| NC | Add robust definitions for telehealth. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove collaborative agreement mandate. |
| ND | Add a definition for telehealth that mentions remote patient monitoring. | Make it clear that a patient-provider relationship can start over any mode. Remove in-person medical evaluation in the North Dakota Food, Drug and Cosmetic Act. | Expand on license by endorsement that only applies to physicians and physician assistants to apply a reciprocity or easy registration to all providers in good standing. | N/A |
| NE | N/A | N/A | Pass an easy registration or reciprocity law for all providers. | Remove 2,000-hour supervision mandate. |
| NH | N/A | N/A | Build on the reciprocity law for physicians and physician assistants to include all providers and put in place an easy registration process for telehealth services. Or expand tele-pass for psychologists to all providers. | N/A |
| NJ | Remove any remaining references in regulation for real-time or video-only telehealth. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | End collaborative agreement mandate for prescribing. |
| NM | Remove interactive requirement. | Update regulations that require face-to-face telehealth visit. And allow prescribing without face-to-face encounter. | Streamline special telemedicine license for doctors, and pass an easy registration or reciprocity law for all providers. | N/A |
| NV | Add definition for remote patient monitoring. | N/A | Streamline Board of Medical Examiners optional special purpose licenses to a registration. Pass an easy registration or reciprocity law for all providers. | Remove two years or 2,000-hour requirement before being able to prescribe controlled substances. |
| NY | Add definition for remote patient monitoring or store-and-forward telehealth. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove collaboration mandate. Remove collaboration mandate, and 3,600 hours of practice requirement before allowing independent practice. |
| OH | Add a definition for telehealth that mentions store-and-forward, and remote patient monitoring. | N/A | Pass an easy registration or reciprocity law for all providers. | Remove collaborative agreement mandate and let NPs practice independently. |
| OK | N/A | N/A | Pass an easy registration or reciprocity law for all providers that moves beyond the subjective process only extended by the Board of Osteopathic Examiners. | Remove supervision mandate and collaborative agreement mandate. |
| OR | Updated to reflect state law. | Make it clear that a patient-provider relationship can start over any mode, and remove prohibitions in regulation that block prescribing over the internet. | Pass an easy registration or reciprocity law for all providers that moves beyond the subjective process only extended to physician. | N/A |
| PA | Add robust definitions for telehealth. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers that extends beyond just the providers from adjoining states. | Remove collaborative agreement mandate and let NPs practice independently. |
| RI | Remove reference in regulation (216-RICR-40-05-1) that states Asynchronous evaluation of a patient, without contemporaneous real-time, interactive exchange between the physician and patient, is not appropriate. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | N/A |
| SC | Add definitions for remote patient monitoring or store-and-forward in the provider code. | Make it clear that a patient-provider relationship can start over any mode. Remove ban on lifestyle prescribing over telehealth. | Pass an easy registration or reciprocity law for all providers. | Remove the written protocol requirement. |
| SD | N/A | N/A | Pass an easy registration or reciprocity law for all providers, and make the physician pathway automatic if they are in good standing. | Remove 1,040-hour practice mandate before being allowed to practice independently. |
| TN | Remove prohibition of remote patient monitoring for provider-based telemedicine. | N/A | Pass an easy registration or reciprocity law for all providers, building on subjective process now only for physicians. | Allow NPs to practice independently. |
| TX | Add definitions for remote patient monitoring and store-and-forward. | N/A | Streamline across-state-line pathway for physicians to just a registration or none. Add universal pathway for all other providers in good standing. | Allow NPs to practice independently. |
| UT | N/A | Allow the provider-patient relationship to be formed using online options, including for prescriptions. | N/A | N/A |
| VA | Update state law to bring clarity on what forms of telehealth can be used to form a relationship and to prescribe. Add formal definitions outside of the statewide telehealth plan for remote patient monitoring and store-and-forward. | Make it clear that a patient-provider relationship can start over any mode. | Pass an easy registration or reciprocity law for all providers. | Remove five-year practice requirement before allowing independent practice. |
| VT | Remove the live requirement for telemedicine. Add definition for remote patient monitoring. Remove requirement for an image for store-and-forward communication. | Make it clear that a patient-provider relationship can start over any mode. | State should expand the across-state-line license and registration to any form of provider, and remove the patient limit and prohibition of care in the state. | Remove the 2,400-hour or two-year collaborative agreement mandate. |
| WA | Remove real-time requirement in the definition of telemedicine, and add definition for remote patient monitoring. | Remove real-time requirement in the definition of telemedicine. | Pass an easy registration or reciprocity law for all providers. | N/A |
| WI | Updated to reflect current state law. | N/A | Pass an easy registration or reciprocity law for all providers. | Allow NPs to practice independently. |
| WV | Add definition for store-and-forward. Remove established patient category to remove face-to-face requirement. | Remove interactive and real time requirements to establish a patient-provider relationship. | Remove prohibition from seeing a patient in state, and allow patients to see across-state-line physicians from other states without requiring them to first be licensed in West Virginia. | Remove three-year collaborative agreement mandate for prescribing. |
| WY | Add a uniform definition for telehealth that makes it clear that synchronous, asynchronous, remote patient monitoring and store-and-forward are allowed. | N/A | Pass an easy registration or reciprocity law for all providers. | N/A |

Stay Informed
Sign up to receive updates about our fight for policies at the state level that restore liberty through transparency and accountability in American governance.


